by Tracy Oostema, PT, DPT, and Kristina Simpson, PT, MSPT
“I want to walk.”
For individuals with acute spinal cord injuries (SCI) embarking on their rehabilitation journey, this is often their primary goal. As physical therapists, it is our challenge and privilege to guide patients in pursuit of their goals and to facilitate recovery of locomotion whenever possible. Considering incomplete tetraplegia and paraplegia account for approximately two thirds of new SCI annually, this is a reasonable goal for many of our patients.1 However, given the degree of impairment many individuals initially experience, including significant weakness, cardiovascular and respiratory deficiencies and spasticity, the process of achieving the end goal of functional ambulation can be daunting. While advances in rehabilitation technology create new possibilities and offer great hope, determining the most efficacious interventions for individual patients while encountering trends for shortened inpatient rehabilitation length of stays1 presents a great challenge for the neurological physical therapist. As such, therapists must be informed about current rehabilitation technology and utilize critical decision-making to guide patients on a successful path toward recovery of ambulation.
The method and progression of gait training varies as much as our patients are individuals. With regard to selection and implementation of technology, there is no particular algorithm, sequence, starting line, or launch pad to over-ground ambulation. Progression is not always unidirectional; at times patients benefit from returning to equipment used previously with a different approach. Some patients require minimal technology to resume ambulation; others have needs that are best met with the use of multiple devices. Regardless of the approach, therapists must always consider maximizing patient participation while maintaining safety and weighing precautions, co-morbidities, and personal factors. Therapists must also be vigilant to perform ongoing assessment of patient response, engagement, and progress to determine when to advance beyond the equipment, with the end goal always being functional over-ground ambulation.

Lindsay Jensen, secured in a harness, works with Tracy Oostema, PT, DPT, on dynamic standing balance using a body weight support system at Mary Free Bed Hospital.
Standing Frames Offer a Starting Point
You have to stand before you can walk. For patients who are particularly weak or deconditioned, the journey to resuming ambulation starts with intense standing work. Standing frames are relatively affordable and thus more widely available to rehabilitation facilities. They are adjustable to accommodate most patient weight capacities, present a very low risk for falls due to a variety of safety features which block joints and prevent movement, and can be accessed through both sliding board and mechanical lift transfers. Among the studies devoted to exploring the benefits of standing, several have investigated the effects of standing on bone mineral density, hip stability, and pressure relief through repositioning. Several of these studies have reported positive outcomes associated with the use of standing systems, including range of motion as well as the psychological benefits of being able to interact with others at eye level. Without the need for a harness, they are compatible for patients with spinal orthoses, and they transition quickly from standing to sitting for patients experiencing orthostatic hypotension. Therapists can use these devices for training cardiovascular tolerance to upright and for pre-gait activities, including sit-to-stand and strengthening of the trunk and lower extremity extensor muscle groups, which can carry over to improved postural control and stance phase of gait, respectively. However, standing frames offer no means to strengthen flexor groups or retrain swing phase of gait, limiting their purpose to stand training only.

Lucas Hernandez, accompanied by Kristy Simpson, PT, MSPT, works on ambulation using a robotic exoskeleton to assist in the swing phase of gait due to neurological weakness.
Robotics and Locomotion
Human locomotion is complex. When retraining patients with acute SCIs, manually facilitating steps that resemble normal gait can be a costly, labor-intensive, and injury-provoking task, particularly for those with profound lower-extremity weakness and spasticity. Robotic body weight-supported treadmill training (BWSTT) is a favorable modality for early mobilization of acute SCI patients who would otherwise require a great deal of physical assistance. These devices generate a physiological gait pattern throughout the lower extremities and with adequate loading of the limbs can activate locomotor central pattern generators2 with the goal of propagating motor recovery. Evidence suggests that robotic BWSTT may be more beneficial for acute SCI patients than traditional over-ground gait training in increasing functional mobility and independence with gait.3
As a clinician incorporating these devices, basic competencies demand proper patient setup and limb loading. Less inherent is the necessary degree of therapist involvement to engage patients and maximize motor output. Therapists challenge swing and stance phase mechanics by reducing the orthosis driving force, and encourage patient effort with verbal and tactile cues, obstacle negotiation, bio- and augmented feedback. Even with highly skilled therapists, patients just don’t work as hard using robotics4 and they don’t allow for variable practice, which is a key principle of motor learning.5 As such, when patients are capable of advancing to gait systems with greater degrees of freedom, they should.
Treadmill-Based Gait Training
We learn from our mistakes. Where robotic BWSTT doesn’t allow a patient to make them, treadmill-based gait training systems with dynamic body weight support (BWS) provide a safe environment for advancing gait, eliminating the risk of falls, offering therapists an eye-level view for gait analysis and an ergonomically friendly space to manually assist. These systems permit patients to deviate from normal gait, correct mistakes, perform at a higher skill level and, through the process of error augmentation, facilitate motor learning for recovery of ambulation.5,6 Manual-assisted BWSTT systems can accommodate highly impaired individuals although significant physical assistance may be necessary at the trunk and lower extremities to facilitate stepping, requiring increased personnel and support. For less-impaired patients, therapists can facilitate higher step intensity with increased speeds, challenge balance by freeing the upper extremities, generate lower limb propulsion with incline walking, and improve stance phase stability through maximal limb loading. Clinical judgment is required as therapists must consider acceptable degrees of deviation from a kinematically normal gait pattern, weighing concerns for joint integrity and potential injury. Therapists must also avoid adverse manual cues such as contact or quick stretch on antagonistic muscle groups. BWSTT systems are beneficial for training a wide continuum of incomplete SCI patients, but as with all equipment, they may precede but certainly must not supercede eventual over-ground training.
Over-Ground Options
Eventually, the feet must hit the ground. With all the technology available, the benefits of over-ground training cannot be overlooked. Over-ground ambulation permits the therapist to challenge postural control, balance, and introduce an assistive device. For the patient who still requires assistance for stance or swing phases of gait, a robotic exoskeleton can be a preliminary transition to over-ground walking. Robotic exoskeleton technology can provide gravity-supported ambulation while engaging the patient to initiate swing and stance phases of gait. It challenges postural control in an upright position without a harness. With exoskeleton software, clinicians can assist or challenge patients in all phases of gait using programmable variable assistance, independently control right and left lower extremity parameters and train functional ambulation tasks such as ramps, curbs, and non-level surfaces in a supportive environment. Additionally, the patient can control speed, stride length, and step height with variable assistance from the orthosis. With programmable exoskeletons, clinicians apply principles of motor learning throughout the gait cycle to facilitate neuroplasticity and improve gait kinematics.
Dynamic BWS systems with track offer similar technology to treadmill-based systems, including the ability to adjust BWS to maximize success and fall-prevention technology, which bolsters safety and patient confidence. They are advantageous for early stand training and allow for progression to over-ground walking, incorporating assistive devices as needed. Furthermore, these systems allow therapists to challenge a patient’s static and dynamic balance, address stepping strategies, manage obstacle courses and barriers, and even negotiate stairs. However, with patients at ground level these systems are less ergonomically conducive to therapists manually assisting. Without the treadmill driving movement, step intensity often is decreased and distance may be limited by track length.
Sometimes, less is more. Some patients only need a safety harness; one step above a good old-fashioned gait belt. An overhead track with harness is a relatively simple device, and while these systems don’t provide BWS or unloading, they can lift anxieties for patients and therapists alike, providing a reliable safeguard from falls. They are a viable solution to support less-impaired patients standing for the first time, or to progress seasoned patients toward stepping without the support of assistive devices. They allow therapists to take a hands-off approach and step back for real-time gait analysis that is not possible while manning a gait belt.
Good Decisions Beget Good Outcomes
No technology can replace the human brain. While high-tech devices are appealing to our patients, no piece of technology for gait training is better than the clinician using it. These devices are therapeutic tools, and when placed in the hands of a therapist who carefully considers clinical decisions, incorporating evidence-based practice, they are valuable assets for promoting neuroplasticity and maximizing patient outcomes, particularly the recovery of locomotion. And at the end of the rehabilitation journey, there is no greater satisfaction for patients and therapists alike than a goal met. RM
Tracy Oostema, PT, DPT, is a physical therapist at Mary Free Bed Rehabilitation Hospital, Grand Rapids, Mich, where she has primarily treated patients with SCIs for the past 11 years. A graduate from Northwestern University Feinberg School of Medicine, her professional interests include gait training patients with incomplete SCIs and PT student mentoring and teaching.
Kristina Simpson, PT, MSPT, is a physical therapist at Mary Free Bed Rehabilitation Hospital, Grand Rapids, Mich, where her practice for the last 15 years has focused on rehabilitating individuals affected by acute and chronic SCI. Gait training after incomplete SCI is a clinical passion and the area in which much of her continuing education has been focused. For more information, contact [email protected].
References
1. National Spinal Cord Injury Statistical Center Spinal Cord Injury. 2017 Facts and Figures at a Glance. Available at: https://www.nscisc.uab.edu/public_pages/FactsFiguresArchives/SCI%20Facts%20and%20Figures%20at%20a%20Glance%202017.pdf. Accessed June 1, 2018.
2. Duysens J, Van de Crommert HW. Neural control of locomotion; The central pattern generator from cats to humans. Gait Posture. 1998;7(2):131-141.
3. Nam KY, Kim HJ, Kwon BS, Park JW, Lee HJ, Yoo A. Robot-assisted gait training (Lokomat) improves walking function and activity in people with spinal cord injuries: a systematic review. J Neuroeng Rehabil. 2017;14(1):24.
4. Israel JF, Campbell DD, Kahn JH, Hornby TG. Metabolic costs and muscle activity patterns during robotic- and therapist-assisted treadmill walking in individuals with incomplete spinal cord injury. Phys Ther. 2006;86(11):1466-1478.
5. Shumway-Cook A. Motor Control Theory and Practical Applications. 1st ed. Baltimore, MD: Lippincott Williams & Wilkins, 1995:23-45.
6. Marchal-Crespo L, Michels L, Jaeger L, LÓpez-OlÓriz J, Reiner R. Effect of error augmentation on brain activation and motor learning of a complex locomotor task. Front Neurosci. 2017;11:526
Gait Trainers Play a Supporting Role for Children with Cerebral Palsy
by Frank Long
The ability to walk substantially impacts quality of life and the ability to navigate the community. For individuals who are affected by a movement disorder such as cerebral palsy (CP), technology may offer a solution for therapeutic interventions that can help support independent ambulation. Gait trainers are a technology that can be helpful to young children affected by CP who want to ambulate independently. Before recommending these devices, therapists should have a clear understanding of the functions they provide and the outcomes that reasonably can be achieved.
Joe Winegar, PT, a physical therapist on the inpatient Pediatric Program at Mary Free Bed Rehabilitation Hospital, Grand Rapids, Mich, is board-certified by the APTA in Pediatric Physical Therapy. His extensive work with pediatric patients has deepened his understanding of the needs of this population, and provided him insight into the role gait trainers can play in serving some of those needs.
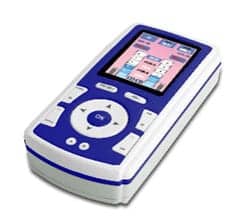
In describing gait trainers, Winegar says, fundamentally they are a type of walker that has four wheels and provides pelvic, trunk, and arm support for the user.
“There are two basic gait trainer designs,” Winegar explains. “One type operates in a reverse walker style and the other type as a forward walker. Their primary use is to provide support to the body from the pelvis up, so that a user with significant motor and neurological impairments can ‘walk,’ using the movements of their legs.”
Usually this walking is not functional in the sense that the person uses it as a means of mobility in the home or community, Winegar says. More likely, he notes, it is part of a program to provide exercise, weight bearing, improve range of motion, and to provide psycho-social benefits through participation. Winegar adds that while gait trainers have proved to be beneficial for many children with cerebral palsy who receive therapy as part of their program in a developmental center, their use with adult populations has been limited.
“These devices are most common in a school setting, specifically in developmental centers that serve children with significant impairments,” Winegar says. He adds that the most common user would be a child with cerebral palsy who is classified as level IV under the Gross Motor Function Classification System.1 These are children, Winegar says, who do not walk functionally and are usually pushed by others in a wheelchair or use a power wheelchair.
“These children will likely never walk in a functional manner but use the gait trainer as part of a therapeutic program,” Winegar says.
Reference
1. Palisano R, Rosenbaum P, Walter S, et al. Developmental and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997; 39(4):214-23.