
Good Shepherd’s pediatric physical therapy supervisor Amanda L. Kleckner, PT, DPT, CBIS, assists a patient who is using a body weight-assisted device over a treadmill.
by Amanda L. Kleckner, PT, DPT, CBIS, and Kandis L. Jones, PT, DPT, PCS
Many physical therapy interventions studied in adult rehabilitation are now being applied to the rehabilitation of children, which requires minor adjustments and parameter changes. This article focuses on several examples of gait and balance analysis technologies and body weight support technologies used for physical therapy assessment and treatment in the pediatric population.
Analysis and Assessment
In many instances, gait and balance analyses are performed using observation and various outcome measures. However, advances in technology and greater accessibility to technology have provided a well-established means of more objectively assessing and treating gait and balance impairments in both adult and pediatric populations. These gait and balance analysis technologies assist clinicians in recommending treatment type and monitoring implemented treatment’s effectiveness. Furthermore, this technology helps clinicians form a customized and comprehensive picture of the main impairments affecting a child’s gait and balance, and can assist in treatment.
During gait analysis using systems that include mats and videos, the patient is videotaped while walking on a pressure-sensitive mat that assesses dynamic alignment, speed, stride length, foot contact, rotational forces, weight-bearing symmetry, and balance. The measurements gathered quantify the body’s movement, force production and muscle activity while walking, and provide a comprehensive picture of the various factors that contribute to the patient’s gait and movement patterns. This data can be used to measure real-time gait performance, make appropriate corrections for the information gathered, and then measure the impact and effectiveness of the modifications made to a patient’s gait pattern.
Another technology available to assist clinicians in assessment and treatment are computerized balance technology systems. Effective balance requires the integration of information from multiple sensory systems, including somatosensory, vision, cognition, vestibular, and the coordination of motor movements to maintain stable balance. Computerized balance technology systems allow for evaluation of the sensory systems and a patient’s integration of sensory information to help identify and objectively quantify sensory and motor problems related to balance. This information enables the clinician to develop an individualized balance rehabilitation program that is designed to challenge and improve the performance of these balance systems.

Body weight-assisted devices can combine with standard rolling walkers for additional support and stability.
Body Weight Support
Body weight support (BWS) systems are another technology that is being used in the pediatric population to assist with improvements in body structure, function, activity, and participation for both gait and balance training. Dynamic BWS gait and balance training systems allow children and adults with conditions such as cerebral palsy (CP), stroke, and spinal cord injury to perform repetitive practice and motor learning activities needed to drive neuroplasticity with an added sense of safety and security. Dynamic BWS technologies allow physical therapists to challenge a patient’s strength, balance, and functional abilities with less need for constant hands-on guarding or moving of the traditional BWS frame.
The design of the trunk harness and overhead trolley system more easily allows the therapist to access the patient’s trunk and extremities for facilitation. The system’s overhead trolley automatically tracks with a patient, allowing practice of both stationary training such as on a treadmill or therapy ball, and over ground mobility training such as gait or stairs. These features allow the user to safely practice walking, balance, strengthening, and other functional skills in a manner more similar to functional mobility and performance of activities in their homes and communities. Additionally, unlike previous static BWS systems, dynamic systems adjust for the naturally occurring vertical movements that occur during the gait cycle.
Currently, studies examining BWS have focused on showing the effects of a BWS program, mainly with locomotion. However, there is a need for further development of clinical practice guidelines, including ideal dosages and specific protocols developed from studies that include larger sample sizes, randomization into groups, and more homogeneous populations.1 Small-scale and heterogeneous studies have shown BWS technologies combined with treadmill training to be beneficial for children with cerebral palsy, with improvements seen in gross motor function, walking, gait speed, and endurance.1-8 However, at this time, dosage recommendations for BWS treadmill training vary greatly from one to five times per week for 1 to 16 weeks, and for durations of 5 to 120 minutes. Due to the current health care model, it is essential to determine a feasible dosage for families that is clinically effective. This will allow patients to incorporate the appropriate frequency into their routine with confounding factors of school and extracurricular activities. Demonstrating an effective dosage also will assist with insurance reimbursement.
The following patient cases illustrate how BWS gait and balance training has been used and results:
Case Studies
Patient case one: 14-year-old male currently seen for physical therapy with upper thoracic-level incomplete paraplegia secondary to an arteriovenous malformation rupture that led to a spinal cord injury. Prior to this episode of care, he ambulated household distances using reciprocal gait orthoses (RGOs) and a standard rolling walker (SRW). Then we progressed to bilateral knee, ankle, and foot orthoses (KAFOs), a thoracolumbosacral orthoses (TLSO), and a SRW in 2015, and finally, in 2016, he progressed to bilateral AFOs or KAFOs and a SRW.
Rehabilitation: Dynamic BWS is used in sitting, standing, and over ground and treadmill walking to address various strength, balance, and postural impairments. For balance, strength, and posture, the patient sits on an elevated dome ball and reaches outside his base of support (BOS). Emphasis is placed on orienting to and maintaining midline by weight shifting to his right side and performing a posterior pelvic tilt to address asymmetrical muscle strength and posture that have led to the development of spinal scoliosis and increased lumbar lordosis. This posture is carried over into standing and walking with dynamic BWS, allowing him to test his limits of stability and practice trunk righting and postural control without the therapist’s constant facilitation. Using decreasing amounts of dynamic BWS, the patient also works on standing and walking with forearm crutches to decrease his dependence on his upper extremities (UEs) for weight bearing, walking with a more normalized gait pattern, and standing with a more erect posture. Sit to stand, mini-squats, and step-ups with variable amounts of BWS are used for lower extremity (LE) strengthening with proper alignment and form that he is otherwise unable to perform at his current level of strength. BWS treadmill training is incorporated with assistance for LEs to increase stance time, alignment during various phases of gait, and increase step length for strengthening, endurance, and gait training.
Current Status: He is currently working on walking during therapy with bilateral KAFOs and forearm crutches using BWS technology. He relies heavily on his UEs when standing and walking, and has significant scoliosis, increased lumbar lordosis, and right hip dysplasia. Patient is independent for wheelchair mobility; he plays basketball and has personal goals related to posture, core strength, stability, standing, and walking.
Patient case two: 13-year-old female with spastic diplegic cerebral palsy with Gross Motor Functional Classification Scale of III. Patient ambulated with posterior rolling walker and bilateral ankle foot orthotics (AFOs) with a goal to decrease to a forearm crutch.
Rehabilitation: Gait analysis with pressure-sensitive mats and video analysis was used to assess gait with this patient. Analysis revealed her left step length was shorter than her right, and she had less weight bearing through her left side. This analysis was used to drive her rehab with the dynamic BWS for over ground gait training with forearm crutches and to correct gait impairments listed. A challenge for young children with congenital diseases or acquired injuries is they grow up using their arms to correct loss of balance (LOB). These children often do not learn another strategy other than protective extension to regain balance, which can be a difficult habit to break. For this patient, this pattern became self-limiting. She had lack of confidence and fear of falling due to reduced spatial awareness without using her hands on a supportive surface. The use of a fall-free environment to regain body awareness and balance during gait allowed her to trust her fall response.
A particular setting called “target matching” is used to read the location of the BWS system and allow her to visually see her center of mass, place it on a specific target, and hold that weight shift. This also allowed her to use her visual system to enhance her body awareness and increase her proprioception without using her hands. Additionally, during this episode of rehabilitation, the dynamic BWS system was used to train fall recovery techniques and dynamic gait and balance to simulate the school environment, which subsequently increased her confidence.
Current Status: During this episode of care, she decreases her assistive device to a single forearm crutch for long-distance walking and her bracing support to one supramalleolar orthoses (SMO) and one AFO. (Since this episode of care, this patient has returned to using two AFOs secondary to increased hamstring tightness from growth.)

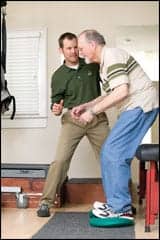
Kandis L. Jones, PT, DPT, PCS, pediatric physical therapist at Good Shepherd Rehabilitation, engages a patient who is using a body weight-assisted device.
Summary of Cases/Clinical Application: The dynamic component of BWS was used with both patients for developing balance strategies and functional mobility that require increased strength, proprioception and postural awareness, and learning fall and recovery strategies. This opportunity is unique for some pediatric clients as they are rarely able to experience and learn balance strategies without using their arms or static external support such as a therapist or support surface. In addition to using this modality for neuromuscular re-education and motor control, some dynamic BWS devices incorporate games or virtual reality in their computer system to allow the patient to engage and for therapists to adapt interventions to their patient’s age. For example, games such as building blocks or ball catch that are activated by the child shifting their weight or squatting to react to a game on a screen can motivate a child to work on therapy goals. A dynamic BWS system also can be paired with other gaming devices, used over a treadmill, elliptical, or with traditional activities such as obstacle courses, puzzles, and toss and catch.
Both cases used dynamic BWS for gait training, motor control, and neuromuscular re-education throughout multiple episodes of care.6,9-12 Due to normal development and aging in pediatric patients throughout years of therapy, their goals and required activities of daily living change. Additionally, the child’s or family’s interests, availability, cognitive level, and motivation may change. At these times, a critical window may develop, and therapists should consider a new episode or period of care. Unfortunately, age and growth can also have a negative impact, as we saw with case two, who required more supportive bracing to maintain her functional status following a growth spurt. This, too, highlights a critical window for therapy where therapists can adapt dynamic BWS parameters to meet the child’s needs.
In conclusion, two patients with different goals and impairments showed improvements in functional status using BWS training as an intervention tool. Using the same modality with different parameters allowed functional improvements during critical windows of care and provided greater confidence to practice challenging skills. Gait and balance analysis technologies can be used to evaluate and treat impairments and functional limitations in both adult and pediatric populations. RM
Amanda L. Kleckner, PT, DPT, CBIS, is the manager of rehab services for outpatient pediatrics at the Health and Technology Center and a physical therapist in pediatrics at Good Shepherd Rehabilitation Network (GSRN), Allentown, Pa. She has been working at GSRN for more than 7 years and is involved with development and use of GSRN’s pediatric technologies for therapy. She also oversees outpatient pediatric rehabilitation services.
Kandis L. Jones, PT, DPT, PCS, is a clinical lead physical therapist in pediatrics at Good Shepherd Rehabilitation Network, Allentown, Pa, where she has worked for more than 3 years. She is involved with the use and implementation of GSRN’s pediatric technologies for therapy, as well as assisting in developing the pediatric physical therapy residency program. For more information, contact [email protected].
References
1. Damiano DL, DeJong SL. A systematic review of the effectiveness of treadmill training and body weight support in pediatric rehabilitations. J Neurol Phys Ther. 2009;33(1):27-44.
2. APTA Section on Pediatrics Fact Sheet. Body-weight-supported treadmill: Using evidence to guide Physical Therapy intervention. 2010.
3. Barbeau H, Visintin M. Optimal outcomes obtained with body-weight support combined with treadmill training in stroke subjects. Arch Phys Med Rehabil. 2003;84:1458-1465.
4. Begnoche DM, Pitetti KH. Effects of traditional treatment and partial body weight treadmill training on the motor skills of children with spastic CP: A pilot study. Ped Phys Ther. 2007;91:11-19.
5. Mattern-Baxter K. Effects of partial body weight supported treadmill training on children with cerebral palsy. Ped Phys Ther. 2009;21:12-22.
6. Novak I, McIntyre S, Morgan C, et al. A systematic review of interventions for children with cerebral palsy: state of the evidence. Dev Med Child Neurol. 2013;55:885–910.
7. Provost B, Dieruf K, Burtner PA. Endurance and gait in children with CP after intensive body weight-supported treadmill training. Ped Phys Ther. 2007;19:2-10.
8. Willoughby KL, Dodd KJ, Shields N, Foley S. Efficacy of partial body weight-supported treadmill training compared with overground walking practice for children with CP: A randomized controlled trial. Arch Phys Med Rehabil. 2010;91:333-339.
9. Bailes AF, Reder R, Burch C. Development of guidelines for determining frequency of therapy services in a pediatric medical setting. Ped Phys Ther. 2008;20:194–198.
10. Christiansen AS, Lange C. Intermittent versus continuous physiotherapy in children with cerebral palsy. Dev Med Child Neurol. 2008;50(4):290-3.
11. Trahan J, Malouin F. Intermittent intensive physiotherapy in children with cerebral palsy: a pilot study. Dev Med Child Neurol. 2002;44(4):233-239.
12. Ustad T, Sorsdahl A, Ljunggren A. Effects of intensive physiotherapy in infants newly diagnosed with cerebral palsy. Ped Phys Ther. 2009;21:140-149.




Hi Amanda and Kandis, thanks for such an informative and interesting article. I am wondering if you have used BWS training as an intervention tool with the spina bifida population and if so, was it successful?
Thank you!
Kim Gregorowicz PT, DPT
Hello Kim, I have used various types of BWS in the spina bifida population and had success. Most recently I used these technologies for “pre-hab” before a spinal rod surgery which hopefully was a precursor to his successful outcome.
Amanda