Effectively managing RSIs can be a daunting task for any therapist. The implications of these injuries run deeper than the subjective complaints of pain and the resultant decline in function reported by patients. Often, the mechanism of injury is a crucial and fundamental component of daily life for these individuals, whether related to work or a recreational activity. The secondary effects of RSI can include decreased productivity in the workplace,1 loss of employment, and financial hardships. It is the role of the hand therapist to perform a thorough musculoskeletal examination of individuals who are affected by an RSI, and cater a plan of care to address the impairments.
Clinical Examination
Repetitive strain injury is a term of causation rather than a tissue-specific diagnosis.2 While patients often present with diagnoses such as lateral epicondylitis or carpal tunnel syndrome, the importance of clinical examination should not be underestimated. Therapists are often afforded the gift of time with patients, and an evaluation can possibly uncover a great deal of information that may have been previously overlooked. A subjective interview should include information regarding general health, job description, MOI, functional limitations, and characteristics of symptoms. Administering an outcome measure such as the QuickDASH is a reliable means of measuring function in patients with upper extremity injuries,3 and the work module is particularly useful for injured workers.
The elbow and the wrist are susceptible to RSI because they are positioned at the distal end of the kinetic chain.4 Hand therapists must thoroughly examine the entire kinetic chain to determine direct and indirect factors contributing to the clinical presentation. Cervical facet joint arthropathy, disc herniations, nerve root entrapments, rotator cuff pathology, and thoracic outlet syndrome may present similarly to distal peripheral nerve injuries and/or tendinopathies of the upper extremity; therefore, screening the cervical spine and shoulder girdle is imperative.5 However, the therapist’s job proximally should not end with
a screen to rule out a diagnosis. When deficits occur proximally within the chain, the elbow and wrist are at risk for injury secondary to increased load transmission distally. Weakness of the rotator cuff and scapular stabilizers, scapular dyskinesis, glenohumeral internal rotation deficits (GIRD), and cervicothoracic mobility deficits are among the proximal impairments that may alter kinematics distally in the upper extremity.4
Examination findings such as range of motion, painful and/or weak manual muscle testing, tenderness to palpation, and joint mobility testing paint a complete clinical picture for the hand therapist. Identifying tests and measures that result in symptom reproduction reveals a great deal of information regarding the affected soft tissues and overall irritability of the injury. Using the example of lateral elbow pain, the clinical examination may reveal the following information: tenderness to palpation at the lateral epicondyle, pain with passive elbow extension and wrist flexion, and weak/painful wrist extension and grip. Based on these preliminary findings, a likely tissue-specific diagnosis is extensor carpi radialis brevis (ECRB) tendinosis. Further special testing should be conducted to rule out arthropathy of the radial head. A quick and simple test, currently being researched at Texas Tech University, is to repeat resisted wrist extension while manually pulling distally on the radius (thus unloading the radial head from the humerus). If the pain significantly decreases, the joint rather than the tendon may be the culprit for the lateral elbow pain.
INTERVENTION
After a tissue-specific diagnosis has been made and impairments have been identified along the entire kinetic chain, a plan for treatment can be established with the goal of returning to the previously injurious activity. Hand therapists have an arsenal of procedural interventions including modalities, splinting, taping, manual therapy, therapeutic exercise, and ergonomic education. Prioritizing interventions based on tissue irritability is of great benefit. For instance, a patient with high levels of pain may require splinting and pain relieving modalities to decrease tissue irritability, whereas an individual with predominantly stiffness and weakness may require joint mobilization and tailored therapeutic exercise.
SPLINTING/TAPING
Patients with highly irritable RSI at the elbow or wrist may benefit from the use of an orthosis to control/prevent motion. Deciding between custom-fabricated and prefabricated splints depends on the acuteness of the injury and the desired goal of splinting. Rigid thermoplastic splints immobilize a joint; therefore, a custom splint may be desirable in the early, inflammatory phase of an RSI. Rigid splinting may be indicated for underlying joint instability that may have precipitated the RSI. Flexible splints and straps will limit motion without strict immobilization. In the case of lateral epicondylitis, use of a counterforce strap during grasping activity can improve maximum grip strength without limiting joint motion.6 To prevent irritation of the radial nerve, hand therapists must limit the use of counterforce straps to pain-provoking activities and ensure patients are not applying them too tightly.5
Therapeutic tape, such as dynamic tape (DT), is an alternative to splinting for many suffering with RSI. By applying DT with the affected musculotendinous structure in a shortened position, the elastic recoil of the tape can reduce loading of the injured tissue during functional activities, thus resulting in less pain with activity.7
THERAPEUTIC EXERCISE
The role of hand therapists includes creating a comprehensive and customized regimen of therapeutic exercise to target strength and endurance deficits noted on clinical examination. A basic understanding of tissue healing is paramount for exercise prescription. An example of this is the initiation of an eccentric strengthening program for the rehabilitation of tendinopathies. Research suggests performing eccentric loading of the involved tissue at a frequency of two sessions per day for 12 weeks contributes to positive outcomes. This is theorized to increase tensile strength of the tendon and destroy immature nerves and blood vessels associated with chronic tendinosis.8
KINETIC CHAIN
Glenohumeral internal rotation deficit is described in the literature as more than 25-degree asymmetry in internal rotation when measured at 90 degrees abduction.9 GIRD has been linked to injury of the upper extremity to include tendinopathy of the elbow. While in the past GIRD was predominantly attributed to tightness of the posterior capsule, there is increasing evidence suggesting the deficits in internal rotation are a result of muscle stiffness that leads to altered scapular mechanics. Restoration of internal rotation via stretching and massage to the posterior rotator cuff muscles, in addition to neuromuscular reeducation for appropriate movement patterns, will help decrease distal stresses at the upper extremity.4
Incorporation of rotator cuff and scapular strengthening within a rehabilitation program for distal RSIs contributes to a stable proximal base of support for all upper extremity function. The concept of whole-body kinetic chain rehabilitation can be taken a step further to include the trunk and lower limbs,4 particularly if the job requires trunk rotation, reaching, climbing, squatting, or lifting.
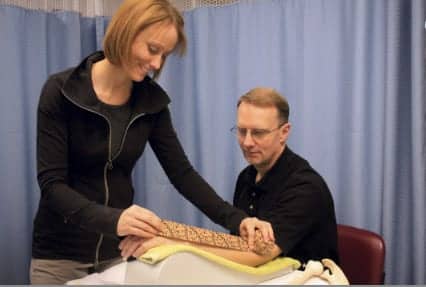
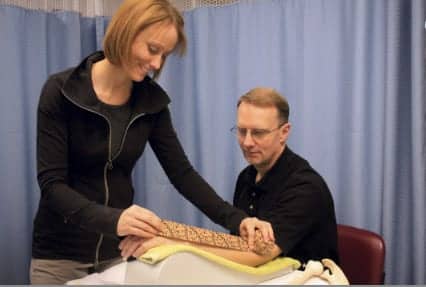
MANUAL THERAPY
Manual interventions can target the joint or surrounding soft tissue. When the RSI involves peripheral nerves, such as carpal or cubital tunnel syndromes, techniques such as neural mobilization should be initiated. The goal of neural mobilization is to maximize excursion and minimize strain on the nerve. Stretching a nerve more than 8% beyond its resting length inhibits blood flow; therefore, it is critical to avoid placing strain on the nerve.10 Rather than tensioning the nerve, the nerve should be moved proximally and distally through the soft tissue as an entire segment, much like flossing. Neural flossing can provide excellent neural mobilization while avoiding stretch.11
Research shows that joint mobilization techniques, such as mobilization with movement (MWM), can increase pain-free grip strength (PFGS) in patients with lateral epicondylitis.12 This is accomplished via lateral glide of the ulna on the humerus with simultaneous grasping and releasing of the hand. Furthermore, mobilization techniques directed at the cervicothoracic spine performed in addition to localized treatments can expedite pain relief and return of PFGS. A lateral glide technique at C5-C6, using the webspace to rhythmically oscillate from the contralateral side toward the painful extremity, has proven beneficial in increasing PFGS and improving pain pressure thresholds in the upper extremity.4
ERGONOMIC EDUCATION
Instilling an understanding of the behaviors that contribute to the RSI is a crucial component of therapy. Educating patients about body mechanics, posture, and injury prevention strategies will decrease the incidence of recurrence. Equipment such as split keyboards and Bluetooth headsets provides simple modifications that can be made to a workspace. If possible, analyzing performance of work tasks can be an opportunity for the therapist to recommend alternative positions or adaptive equipment to decrease repetitive strain on soft tissues.1
SUMMARY
Hand therapists must take the reins as experts in the examination and treatment of RSIs of the upper extremity. Patients look to us for guidance with these debilitating injuries, and it is our responsibility to provide them with education, empowerment, and a comprehensive rehabilitation program addressing impairments along the entire kinetic chain. Our skills of differential diagnosis and a fundamental understanding of tissue healing should remain driving factors in the creation of a treatment plan. The successful return to previously painful activities is tremendously rewarding to both the patient and the therapist. RM
Elizabeth Soika, PT, DPT, CHT, is director of hand therapy for Columbia Rehabilitation Clinic Inc, South Carolina. She earned her CHT in 2006 and achieved a Doctorate of Physical Therapy
in 2008. For more information, contact [email protected].
References
1. Nainzadeh N, Malantic-Lin A, Alvarez M, Loeser AC. Repetitive strain injury (cumulative trauma disorder): causes and treatment. Mt Sinai J Med. 1999;66(3):192-196.
2. Konijnenberg HS, de Wilde NS, Gerritsen AAM, van Tulder MW, de Vet HCW. Conservative treatment for repetitive strain injury. Scand J Work Environ Health. 2001;27(5):299-310.
3. Mintken PE, Glynn P, Cleland JA. Psychometric properties of the shortened disabilities of the Arm, Shoulder, and Hand Questionnaire (QuickDASH) and Numeric Pain Rating Scale in patients with shoulder pain. J Shoulder Elbow Surg. 2009;18(6):920-926.
4. Gibson J. Rehabilitation of the elbow. In: Stanley D, Trail I, eds. Operative Elbow Surgery. 1st ed. London: Churchill Livingstone Elsevier; 2012:511-532.
5. Fedorczyk JM. Elbow tendinopathies: clinical presentation and therapist’s management of tennis elbow. In: Skirven TM, Osterman AL, Fedorczyk JM, Amadio PC, eds. Rehabilitation of the Hand and Upper Extremity. 6th ed. Philadelphia: Elsevier Mosby; 2011:1098-1108.
6. Van de Streek MD, Van der Schans CP, De Greef MHG, Postema K. The effect of a forearm/hand splint compared with an elbow band as a treatment for lateral epicondylitis. Prosthet Orthot Int. 2004;28:183-189.
7. Dynamic Tape: Weapons for serious athletes and clinicians. Available at: http://www.dynamictape.com/content/dynamictape/#.UQWpTRwUUwc. Accessed January 26, 2013.
8. Alfredson A. The chronic painful Achilles and patellar tendon: research on basic biology and treatment. Scand J Med Sci Sports. 2005;15:252-259.
9. Dines JS, Frank JB, Akerman M. Glenohumeral internal rotation deficits in baseball pitchers with ulnar collateral ligament deficiencies. Am J Sports Med. 2009;37(3):566-70.
10. Clark W, Trumble T, Swiontkowski M, Tencer A. Nerve tension and blood flow in a rat model of immediate and delayed repairs. J Hand Surg. 1992;17:677-687.
11. Porretto-Loehrke A, Soika E. Therapist’s management of other nerve compressions about the elbow and wrist. In: Skirven TM, Osterman AL, Fedorczyk JM, Amadio PC, eds. Rehabilitation of the Hand and Upper Extremity. 6th ed. Philadelphia: Elsevier Mosby; 2011:695-709.
12. Pagorek S. Effect of manual mobilization with movement on pain and strength in adults with chronic lateral epicondylitis. J Sport Rehabil. 2009;18:448-57.