In pediatrics, the patients are growing and developing. The equipment ordered today must provide opportunity for physical growth and ideally can adapt to the patient’s future progress.
By Jean Murby, PT, PCS; Christa Rocco, DPT; Kristen Lally, DPT; Marianna DiMaggio, DPT; and Stacey Zalanowski, DPT
Standing and weight-bearing are critical components of a child’s motor skill and musculoskeletal development. Children begin pulling to stand as early as
8 months and begin their cruising phase of walking at 10 months. As pediatric physical therapists, we frequently hear the concerns of parents whose children have neuromuscular impairments asking, “When will my child walk?” Walking is an emotional, proud moment of every child’s development.
A progressive standing program is recommended for children who are nonambulatory by 12 to 18 months to introduce weight-bearing through their lower extremities.1 Research also shows that prolonged standing improves stride length, gait speed, stride time, stance time, and muscle tone.2 This research indicates that a consistent standing program can have profound effects on a child’s gait. The ease and ability to complete a standing program should be a focus for pediatric patients’ long-term health and mobility.
In order to stand and walk, many children with neuromuscular impairments require equipment. In 2010, close to 50% of children with special health care needs required more than five services or pieces of equipment over that year. Of these same children, 4% needed mobility devices and 11% needed durable medical equipment over that year.3 Today, there are many choices for pediatric mobility equipment.
Let’s consider a patient scenario. Jane is a 12-year-old with a history of developmental delay who presents to an inpatient rehabilitation hospital 2 weeks after surgical fixation of her scoliosis. Prior to the surgery, she was walking without physical assist or equipment but with some gait deviations. Currently, she is maximal assist with two people to stand up for 2 minutes. Jane is tolerating 20 minutes in a stander daily. Jane is dependent for walking using a robotic gait training device. Jane has trialed a gait trainer only once, she was dependent with two people. Jane’s functional progress toward her walking baseline ability has been slow since her surgery due to impairments in strength, endurance, and pain. Jane is going home with her parents in 2 weeks and you, as the physical therapist, are preparing your equipment recommendations and ordering.

In pediatrics, the patients are growing and developing. The equipment ordered today must provide opportunity for physical growth and ideally can adapt to the patient’s future progress.
Let’s consider the following factors related to our case:
Patient/Family Desires: Her parents really want Jane to be walking again, and they want a gait trainer ordered. Due to communication and cognitive issues from her developmental delay, Jane isn’t able to express her goals.
Therapy Goals: Long-term therapy goals are to encourage progress toward her baseline walking ability. You have reached out to both her school and outpatient physical therapists. They have a variety of standers and gait trainers that Jane can access during school and during her outpatient therapy sessions.
Economic Factors: Pediatric mobility devices can cost up to $5,000, but range from $1,000 to 5,000.4,5 The cost of these devices may be covered in a variety of ways. For those with insurance, coverage for the equipment depends on the type of insurance, the type of device, and whether the child’s mobility situation meets the requirements for coverage.6 In addition, usually only one piece of mobility equipment is covered. Also, health plans may place fairly low limits (eg, $1,500) on the maximum amount that they will pay for assistive equipment during a year. They may also limit how often they will pay for an item (eg, once every 5 years).
It is estimated that almost 5% of children with special health care needs are uninsured.5 If the child is uninsured or their insurance health plans deny payment for these devices, the options are not obtaining the equipment, family self-paying, or seeking an external funding source. Public funding allows children to have resources available to them to help them succeed at their schools. In all of these coverage options, stress about finances occurs. More than 20% of families who have children with special health care needs reported financial problems due to their child’s health condition in 2010.5
EQUIPMENT/VENDOR TRIAL
Another requirement for coverage is the occurrence of a successful trial of the specific mobility device being ordered. Gaining access to the equipment in a timely manner can be challenging. Also, families might want to consider how the devices may collapse for storage in the home and transport in the car. They may also want to consider options to move the stander from one location to another, such as a mobile base.7
Developmental factors: In pediatrics, the patients are growing and developing. The equipment ordered today must provide opportunity for physical growth and ideally can adapt to the patient’s future progress.
It may be helpful to consider the advantages and disadvantages of the types of pediatric mobility equipment.
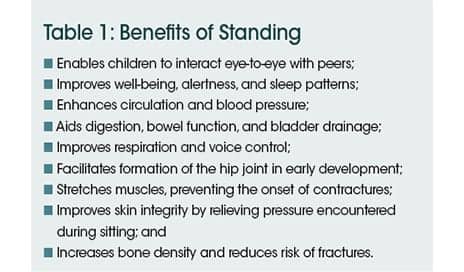
First, let us consider standers. In addition to the benefits of standing as noted in Table 1, standers provide support for improved alignment, visual interaction with the environment and peers, and hand-eye coordination opportunities. Tray support allows the child to use both upper extremities to further assist with head and trunk righting. Other accessories can improve patient’s alignment depending on their needs, including footplates that can accommodate leg length discrepancies,8 hip guides, lateral trunk guides, adjustable angle footplates, and the ability to adjust to a child’s growth. Some children may not tolerate full upright positioning due to weakness or range of motion restrictions. This positioning can cause decreases in lower extremity weight-bearing. Other alterations in weight-bearing may occur during stander use due to angle of inclination, use of prompts, and inconsistent positioning by different caregivers.9
STANDER TECHNOLOGY OVERVIEW
Advantages of prone standers:
• Facilitate head and trunk postural control and righting.
• Can offer variable footplate angles to accommodate increased muscle tone or contractures.
• Provide varied vertical angles for progression of upright standing.
Disadvantages of prone standers:
• Prompts and straps may be challenging for caregivers to adjust for optimal positioning.
• Transfer onto device will be a dependent lift.
• Actual weight-bearing through bilateral lower extremities can show a variance with caregiver positioning and the angle of stander.9
Jane does not require all the supports of a prone stander.
Advantages of supine standers:
• Provide posterior support for improved trunk and head control.
• Provides support for patients with low tone.10
• Slow transition to vertical position provides a great option for patients who may not have stable hemodynamic response.
Disadvantages of supine standers:
• Optimal positioning may be difficult when a child has reduced knee extension range of motion.
• Decreased lower extremity weight-bearing when a child has reduced knee extension range of motion, even when contracture is supported by the device.
• To accommodate the child’s growth, the size of the base must increase to maintain safety, making the footprint even larger.
• Reduced weight-bearing forces through the legs when the device is not tilted fully upright.
• Transfer onto the device will be a dependent lift or sit-to-stand transfer.
Jane does not require all the head and upper trunk supports of a supine stander.
Advantages of “sit-to-stand” standers:
• Facilitate the sit to/from stand transition.
• Provide progressive weight-bearing through lower extremities throughout the transition to stand.
• Ease of transfer onto the device, transfer can be a squat pivot or slideboard.
• Compact footprint for use in home.
• Allow for independent use as appropriate.
• Some models allow for reciprocal movement of lower and/or upper extremities, which may allow prolonged tolerance to standing, more muscle activity, and more aerobic benefits.
• Provide the ability to progress to more active participation.
• Knee blocks can be loosened to engage more quadriceps activity to maintain static knee extension.
• Chair angle can be decreased to engage more static quadriceps and gluteal activity to maintain full upright standing.
• Chair angle can be decreased to engage more dynamic quadriceps and gluteal activity during transitions from partial to full standing, and eventually from full sitting to full standing.
Disadvantages of “sit-to-stand” standers:
• Requires head and trunk control for optimal upper body posture.
• Requires stable hemodynamics in sitting.
Jane is currently using a sit-to-stand stander.
Besides standers, the other type of pediatric mobility devices are gait trainers.
Let’s first consider the question of focusing on a standing program versus gait training. Focusing on a standing program can be an effective way to improve quadriceps and gluteal control. Initiating gait when the patient has little active control in the lower extremities may shift the patient to use compensatory strategies such as using the upper extremities for offloading their body weight and using trunk control to advance their legs. Prolonging focus on standing before initiating gait can be beneficial in these patients. They can strengthen their extensor muscles and then learn to use the correct muscles during stance phase of gait. Therefore, it can be more effective to focus on achieving and maintaining standing before working on gait. Allowing patients to walk in their environment is the main benefit of gait trainers.
GAIT TRAINER TECHNOLOGY OVERVIEW
Advantages to a gait trainer with a “saddle” or “pony”:
• Provides greater support for a child who cannot support themselves fully through their legs.
• Allows for free movement of legs through unloading mechanism.
• Ease of set up, child sits on the saddle during set up.
• Allows for seated breaks on the saddle or pony as the child progresses to fully supporting themselves through their legs.
Disadvantages to a gait trainer with a “saddle” or “pony”:
• Limited weight-bearing through legs when sitting on the saddle.
• Tendency for children to sit on the support, even when not needed.
Jane has not trialed a saddle gait trainer. She will likely remain seated throughout gait training and requires more upper trunk support.
According to a recent nationwide survey completed by randomly selected members of the Section on Pediatrics of the American Physical Therapy Association (APTA), gait trainers with soft fabric hip positioners/ pelvic harnesses are one of the most commonly used gait trainers.
Advantages of gait trainer with pelvic harness:11,12
• Can easily be switched to/from an anterior to a posterior facing device.
• Large base provides stability for patients with significant balance impairments.
• Various prompts, from the child’s upper extremities to their trunk to their feet, can be added for support easily and without any tools.
• Various prompts can be removed easily without any tools so that these devices can be used as hand-held walkers.
• Variable weight-bearing through lower extremities during walking.
Disadvantages of gait trainer with pelvic harness:11,12
• Difficult to use in small spaces due to large base, which may limit interaction with peers in a home or school classroom.
• Pelvic harness does not promote the sinusoidal pattern while ambulating.
• Challenging to transport between various environments due to large base even when collapsed.
• Transfer into the device and setup are challenging. The patient has to remain standing while the harness is set up.
• Tendency for children to sit on the support, even when not needed.
Jane has trialed a gait trainer with pelvic harness once. She relied heavily on the harness support throughout gait training, and her upper trunk remained flexed.

One benefit associated with posterior pediatric walkers is that they allow the child to directly approach a peer or the environment without the device being between them.
WALKER TECHNOLOGY OVERVIEW
Advantages of a posterior walker:
• Light and collapsible, making transport between different community activities and places easy.
• Allows the child to directly approach a peer or the environment without the device being between them.
• Full weight-bearing through lower extremities during walking.
Disadvantages of a posterior walker:
• Transfer into the device is by standing up and then turning to face forward, which can be challenging to sequence.
Jane has not tried this device. She requires more support due to trunk and lower extremity weakness.
Advantages of an anterior walker:
• Light and collapsible, making transport between different community activities and locations easy.
• Full weight-bearing through lower extremities during walking.
Disadvantages of an anterior walker:
• For children with crouched gait, it may lead to more crouching with more flexed positioning.
• Does not allow the child to directly approach a peer or the environment without the device being between them.
Jane has not tried this device. She will not do well with this little support from a device.
AN INFORMED DECISION
So back to the question of, “What mobility equipment should we order for Jane?” Ideally, Jane would be best served by having access to a trial of a sit-to-stand stander for a few months at home. After these few months with a continued daily standing program at home, school-based physical therapy, and outpatient physical therapy sessions, a re-evaluation of Jane’s mobility equipment needs could occur. If significant progress occurs, the stander may no longer be needed and a gait trainer could be ordered.
The current situation for pediatric mobility equipment doesn’t allow this type of short-term trial. We would like to provide a few suggestions for making short-term use of equipment more feasible. Rental programs could be established with vendors. Groups providing used and low-cost pediatric mobility equipment could be better organized and easier to access.
Pediatric mobility equipment provides many exciting and beneficial options, but it requires careful consideration of several critical variables, including patient/family desires, developmental level, economic restraints, therapy goals, and provision of successful equipment and vendor trials. RM
Jean Murby, PT, PCS, Christa Rocco, DPT, Kristen Lally, DPT, Marianna DiMaggio, DPT, and Stacey Zalanowski, DPT, are therapists at Spaulding Rehabilitation Hospital, Boston. For more information, contact [email protected].
References
1. Stuberg W. Considerations related to weight-bearing programs in children with developmental disabilities. Phys Ther. 1992;72(1):35-40.
2. Salem Y, Lovelace-Chandler V, Zabel R and Gross McMillan A. Effects of prolonged standing on gait in children with spastic cerebral palsy. Phys Occup Ther Pediatr. 2010;30(1):54-65.
3. US Census Bureau, 2010-2012 American Community Survey. Available at: https://www.census.gov/programs-surveys/acs/data.html. Accessed February 6, 2016.
4. Example of equipment prices. Available at: http://www.rehabmart.com. Accessed February 6, 2016.
5. National Survey of Children with Special Health Care Needs. NS-CSHCN 2009/10. Available at: http://www.childhealthdata.org. Accessed February 6, 2016.
6. Coverage of Assistive Technologies and Personal Assistive Services. In: Institute of Medicine (US) Committee on Disability in America; Field MJ, Jette AM, editors. The Future of Disability in America. Washington (DC): National Academies Press; 2007. Available at: http://www.ncbi.nlm.nih.gov/books/NBK11441. Accessed February 6, 2016.
7. Paleg G. Get Them Standing. Advance Healthcare Network. Published March 31, 2014. Updates 2015. Available at: http://physical-therapy.advanceweb.com/Archives/Article-Archives/Get-Them-Standing.aspx. Accessed January 29, 2016.
8. Hansel R. Embracing Gravity. Advance Healthcare Network. Published January 2, 2014. Updated 2015. Available at: http://physical-therapy.advanceweb.com/features/articles/embracing-gravity.aspx. Accessed January 28, 2016.
9. Herman D, May R, Vogel L, Johnson J, Henderson RC. Quantifying weight-bearing by children with cerebral palsy while in passive standers. Pediatr Phys Ther. 2007;19:283-287.
10. Dobrich L. Making A Stand. Advance Healthcare Network. Published November 15, 2010. Updated 2015. Available at: http://physical-therapy.advanceweb.com/Archives/Article-Archives/Making-a-Stand.aspx. Accessed January 29, 2016.
11. Low SA, McCoy SW, Beling J, Adams J. Pediatric physical therapists use of support walkers for children with disabilities: a nationwide survey. Pediatr Phys Ther. 2011;23(4):381–389.
12. Paleg G, Livingstone R. Outcomes of gait trainer use in home and school settings for children with motor impairments: a systematic review. Clin Rehabil. 2015;29(11):1077–1091.