 |
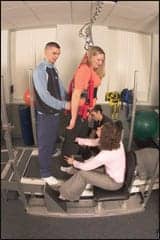
| Caren Sydnor (standing, center) receives locomotor training from therapists at Magee Rehabilitation Hospital in Philadelphia. Magee is an NRN center for the Christopher and Dana Reeve Foundation. |
Some 780,000 strokes are expected to occur this year. In the United States, 160,000 people die annually from stroke, making it the third leading cause of death—and the number one cause of adult disability, according to the National Stroke Association.
A stroke or severe injury can wreak havoc on cognitive and motor functions, but the ranks of survivors number almost 5 million. Significant strides have been made to boost patients’ prospects for functional improvement and recovery. Physical therapists and occupational therapists are on the front lines, helping to restore patients’ independence.
ASSESSING THE DAMAGE
At the 150-bed Burke Rehabilitation Hospital, White Plains, NY, the Fugyl-Meyer assessment is performed on Day 1 by Physical Therapy and Day 2 by Occupational Therapy, evaluating patients’ motor control for UE/LE, range of motion, sensation, ability to know where the limb is in space, and balance. Stroke patients who demonstrate lateropulsion would be evaluated with the Burke Lateropulsion Scale. PTs are looking to see if there is resistance to a patient being brought to midline, because some patients use their strong arm to push toward their weaker, hemiplegic side, says Jennifer Matuszewski, PT, MS, CKTP, advanced clinician of stroke at Burke, who works in an inpatient rehab unit. Patients are graded on a scale of positions: supine, sitting, standing, transfers, and walking. A pulmonary assessment involves auscultation of the patient’s lung fields to see if chest physical therapy is required. Burke also conducts a formal balance assessment, which may include the Berg Balance Scale, and Dynamic Gait Index.
The balance assessment includes testing of the visual system, and in conjunction with OTs, standardized testing is performed, classifying inattention or neglect of one side with tests such as Star Cancellation and Line Bisection. Vestibular assessment evaluates lateropulsion and whether a patient exhibits vestibular hypofunction. Positional tests are performed, such as positional movers for BPPV (benign paroxysmal positional vertigo), and a somatosensory test looks at the patient’s ability to close their eyes and balance on a piece of foam. Burke’s PTs, including Matuszewski, reevaluate baseline assessment data daily and chart a weekly or status progress note, reevaluating formal tests and measures and whether the patient is expected to meet set goals.
Burke’s PTs sometimes accompany OTs on a home visit, evaluating transfers, ambulation, stair negotiation, entrances, and exits, to augment the OT home safety evaluation and recommendations. Matuszewski says PTs may sometimes teach alternative methods for descending stairs, such as sidestepping, and they may have to determine options for negotiating stairs if a device is needed to supplement the handrail. Family and caregiver training often dovetails into the process, preparing helpers for what lies ahead.
Once-familiar home terrain may harbor hazards for someone whose mobility is impaired. “Most falls occur in the home and environments people are comfortable with,” says Cheryl Maurer, PT, MS, CPed, founder of Functional Mechanics, Watertown, Mass. People tend to let their guard down at home, but Maurer’s tips can help restore the safe haven.
- Adequate illumination that fosters even lighting is essential.
- Tack down fringed throw rugs and remove the fringe; remove the lip on thresholds.
- Move slowly and segmentally when arising from bed to ensure alertness, and avoid yielding to momentum.
- Position a commode or a urine bottle (for men) bedside, and place a disposable nighttime pad atop the sheet for quick cleanups.
INTEGRITY OF THE BALANCE RESPONSE
Maurer, a certified pedorthist who specializes in foot and ankle dysfunction, alters the foot-ground interface with shoe modifications, custom shoes, bracing, custom orthotics, or other actions—such as retraining motion, strength, and patient awareness. Physicians may urge patients to wear a relatively soft shoe—especially those who do not have normal feeling in their feet—but she says that may worsen balance. “If you were standing on a pillow, that pillow is moving underneath you and you don’t have good awareness of where you are,” Maurer says. “If you’re on something that’s a little bit firmer—it doesn’t have to be rigid—you have a better sense of where you are.”
People may need to shuffle to know where they are in space and reinforce their stability. An athletic shoe can cause the wearer to stop short or tumble. An SAS or an Easy Spirit-type shoe with a rubber sole may offer the right amount of grip and does not tend to get caught on a rug or floor if someone shuffles—with a seasonal caveat. It does not provide needed traction when leaves litter the ground or rain-wet leaf debris fills sidewalk cracks, or if slush is present. “This is a really dangerous time of year. It is … just shy of walking on ice,” says Maurer. In those conditions, she suggests a shoe with a more aggressive outsole—such as an athletic walking shoe that helps grab through the dirt and dumps dirt back on the pavement, like a snow tire. The smoother, rubber-sole, SAS-type shoe works better in the home, she says.
A weapon against winter’s mush—Yaktrax (www.yaktrax.com)—was featured in a study published by the Journal of Gerontology. Maurer says the crisscrossing rubber straps larded with metal, which are strapped underneath the shoe to grab into the snow and the ice, help reduce falls.
Patients also need to be aware of how far things project off of their bodies. Those who are fitted with an AFO need to wear a larger-size shoe to avoid catching the shoe climbing stairs or entering/exiting a car, Maurer says.
Balance is also controlled by images and retinal slip, as motion flits across the retina, and the motion needs to correlate with feedback from the vestibular system. If the information is not tracking correctly, a patient may perceive that the world is spinning or something is going to happen, and the body will reflexively respond. “You have to change or create a different environment or perceived environment for the body to come out with a different way of producing motion,” she says. This can be done through retraining or learning coping methods.
INSURANCE REIMBURSEMENT
Many stroke patients are older than 65 and are insured by Medicare. While a patient’s length of stay is based on medical necessity, various factors—including a patient’s presentation, functional status, and medical comorbidities—contribute to the formulation of a discharge date.
Stroke patients may also be case managed by an insurance company. Initial assessments and periodic updates from the patient’s medical record are periodically faxed by the hospital’s social work case manager to a nurse case manager at the insurance company. The therapy documentation is used to justify a patient’s need for acute rehabilitation. Insurers may determine that a patient no longer needs an acute rehab level of care, and that another level of care is more cost-effective. Family training by therapists is necessary to ensure a patient’s safe discharge home. A patient’s physician makes the final decision regarding a patient’s discharge from the hospital.
Burke generally uses the functional independence measure (FIM), grading patients on their transfers, walking, social interaction, problem solving, and memory. Those numbers, and the physician’s and therapist’s recommendation, coalesce into a discharge plan and a specified length of stay, which may be amended, depending on the results.
TECHNOLOGIES/MODALITIES USED DURING TREATMENT
Some of Maurer’s patients use crutches because they have drop foot or back issues, and others have problems with their arms, such as ulnar nerve entrapment. Some crutches are designed with a spring, which helps absorb impact, and an angled tip. The handles are ergonomically angled properly for the wrist.
Melanie Garrett, PT, who works in outpatient rehab at Baptist Health Care, Pensacola, Fla, relies on some low-tech options, such as a knee-stabilizing air cast and a long-leg immobilizer. She creates a sling with the Thera-Band and inserts a stacking-type cone, running it through the holes in the cone and gripping the patient’s hand around the cone; she drapes the band around the patient’s shoulder like a sling or a one-sided backpack. PTs could tie the Thera-Band to a belt loop, creating desirable tension, so when patients take a step, the Thera-Band springs and swings the leg through.
Bill Thornton, MPT, teaches courses and conducts research at Wayne State University, and for 3 years has been working with a vibration plate called the Wave. He says it offers great benefits for those who have had a stroke, brain injury, or spinal cord injury—namely, reduction in spasticity and increased muscle activity. “If I can position you on it correctly and turn it on, I can get the muscle to activate,” he says. He recently became a consultant for the company that produces it. He works at Irvine Head Injury Inc, Southfield, Mich; Rehabilitation Medical Specialists, Southfield; and the Center for SCI Recovery, the Rehabilitation Institute of Michigan (RIM), Detroit and Grand Rapids.
Thornton is seeking the purest vertical vibration, and the Wave vibrates up to 4 mm. “I will guarantee it will rattle your teeth if positioned wrong. It’s very intense,” he says, noting the device is win-win for the therapist too. “Whether it’s just improved motor activation, improved sensation, or really looking at being efficient with your workload.”
The Second Step system allows earlier ambulation of stroke and other neurologically compromised patients by creating a virtually fall-free environment, says Lisa Stevens, PT, senior therapist at the Brain and Spine Recovery Center at Brackenridge Hospital, Austin, Tex. “While it may still take two or even three therapy staff in the most involved cases, initiating stepping as early as possible is critical to ultimately achieving functional gait,” she says. “I was able to manually pattern symmetrical gait in hemiplegic clients while the device provided a firm forearm resting surface for upper-body support and extended the time tolerated for practicing locomotion.” With the framework and the harness, she was able to move straight to standing and limited gait instead of being stuck in transfer training for the first day or two, she says. It makes the process possible from the bedside, which allowed the staff members to work without a dedicated gym space when necessary.
At Burke, functional electrical stimulation (FES) helps with foot drop, or dorsiflexion. Up-and-coming nerve-stimulation technologies include the WalkAide, FES for dorsiflexion. The LiteGait is a portable body-weight-support device with a harness system that takes weight off of patients, so they can perform standing activities and walking with the device. Matuszewski incorporates a lot of neuromuscular reeducation and gait training within treatment sessions. The facility uses assistive devices—canes, walkers, and a hemibar or a unilateral bar—with patients who are plegic or paretic on one side. Training without devices is also practiced to facilitate neurorecovery.
Burke incorporates the Nintendo Wii in balance training, in cardiac training, and as an aid in visual coordination. The facility also uses upper extremity robots—for shoulder, elbow, and wrist—developed at MIT, which resemble a sophisticated version of the old Atari games’ visual screen and feedback. The robot takes patients, via a joystick, through the range of motion. Patients provide the effort, and the machine matches the effort and backs off as the patient completes the range of motion.
Locomotor training is a rehabilitation intervention built on scientific evidence—activity-dependent plasticity, says Susan Harkema, director of the NeuroRecovery Network, funded by the Christopher and Dana Reeve Foundation. “That’s a basic neuromechanism,” she says. “But when you come into the physical therapy, occupational therapy environment, what it tells us is that the nervous system is constantly changing.” Harkema is an associate professor in neurosurgery and the director of research at Frazier Rehab Institute, Louisville, Ky, and also the rehabilitation research director at the Kentucky Spinal Cord Injury Research Center at the University of Louisville.
The principles are just being introduced to rehabilitative environments, and while much is still to be learned, Harkema says the nervous system will continue to change even years after a stroke or a spinal cord injury, and the possibility remains of guiding the change to be more functional.
Judy O’Rourke is associate editor of Rehab Management. She can be contacted at .
Locomotor Training
Locomotor training is a rehabilitation intervention built on scientific evidence-activity dependent plasticity, says Susan Harkema, director of the NeuroRecovery Network, funded by the Christopher and Dana Reeve Foundation.
Harkema says the accepted wisdom used to be “Here’s your injury. This is where you are, and there’s not much likelihood of you improving. And so we’re going to teach you how to compensate.” A sea change has occurred, she says. “What scientifically we now know … is that if you train an individual over and over and over again in a specific task, even the injured nervous system-whether it’s a stroke or a spinal cord injury or some other neurologic disorder-can learn from that experience,” she says. “Injury to the brain, or injury to the spinal cord that loses information from the brain, doesn’t prevent the nervous system in the spinal cord from relearning.”
The Network operates seven facilities across the country, aiming to support specialized centers that focus on evidence-based and activity based therapies. Their practices are standardized, so they are consistent, and detailed outcome measures are recorded to evaluate the program. “That mission was really because of the vision and dedication of Chris and Dana Reeve,” Harkema says. “Chris came to the laboratory at UCLA many years ago when we were just really discovering that these mechanisms did exist in the human spinal cord. His vision was, ‘I can come here and get cutting-edge interventions; how do we make it more accessible to people across the country, regardless of where they live or what their socioeconomic situation is? How do we get this knowledge out to people and access to people more quickly?'”
The remaining pathways can functionally reorganize. Harkema likens the process to the highway system. “You can get from the west to the east on the 10, but if the 10 is shut down somewhere, you still can get there, but it’s going to be by an unknown route, and it’s going to take longer. But more and more, if you have to drive back and forth, you’re going to get more efficient at that route.” Harkema is an associate professor in neurosurgery and the director of research at Frazier Rehab Institute, Louisville, Ky, and also the rehabilitation research director at the Kentucky Spinal Cord Injury Research Center at the University of Louisville.
In a stroke, there is not complete loss of communication between the brain and spinal cord, and in a spinal cord injury, it is probably rare to have a complete loss of connections, she says. By retraining the nervous system, using activity dependent plasticity, certain connections can be strengthened. “So, you can actually change what that functional output is. And it’s not completely dependent upon the brain. And that’s sort of the new finding. That’s what we’re adding to the repertoire of physical therapists.” The former top-down approach-of figuring out how much brain function remains and tapping it or compensating for a deficit-has morphed into: recovering what appears to be a deficit via the neuromechanism of activity dependent plasticity, which has been translated into a clinical term: activity based therapy. “This means you activate the nerve system below the level of injury or the affected part of the nervous system,” Harkema says. “So, in a stroke, for example, it means you activate the arm that’s affected, you activate the leg that’s affected versus compensate for it.”
One way to do that, specifically for standing-walking, is locomotor training. The spinal cord is very complex, and it can forget, remember, relearn, and make decisions, Harkema says. And it can integrate complex information, such as the position of the leg, or whether a muscle is contracting, or whether the patient has weight on one leg or both legs. With that information-even if the person doesn’t recognize it like they did before a spinal cord injury or stroke-the spinal cord itself, especially in stroke, still gets the signals and can interpret them. If patients practice walking with the right cues, such as walking at a normal walking speed with the right kinematics of the legs, flexion, extension, alternating weight-bearing, and they do it over and over and over again, the networks of the nervous system and their connections, will be optimized to do it better, she says.
“We just started implementing these concepts,” Harkema says of the Network. “We’re just beginning to scratch the surface of the efficacy, or which patients would most benefit, or what’s the best way to do it.” The principles are just being introduced to rehabilitative environments, and while much is still to be learned, Harkema says the nervous system will continue to change even years after a stroke or a spinal cord injury and the possibility remains of guiding the change to be more functional.