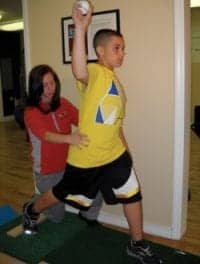
Photo Caption: The Young Stroke Program prepares stroke survivors of all ages for a return to baseline. Stroke survivors who were very active prior to their stroke are often ready, willing, and able to participate in a more focused, rigorous program to help them return to the life they led pre-stroke. Here, a patient practices cooking skills. Photo: Karen Ingham Photography
by Stephanie Zanvettor, PT, CBIS, CCI
Every year, nearly 800,000 Americans are faced with the challenge of recovery after a stroke.1 While the majority of strokes occur in people aged 65 and older, the incidence has been increasing in adults aged 49 years and younger over the last three decades. This can potentially be attributed to the fact that risk factors for stroke such as high blood pressure and type 2 diabetes have been on the rise among younger and middle-aged adults.2 In 2014, nearly 40% of people hospitalized for stroke were less than 65 years old.1
With a keen understanding that recovery and rehabilitation is not a one-size-fits-all solution for those who led an active life before their stroke, the medical and rehabilitation staff at Gaylord Specialty Healthcare—a Connecticut rehabilitation-focused healthcare system with CARF specialty accreditation for its stroke program—launched the Young Stroke Program to give this generally younger and more active segment of stroke patients the customized, rigorous care needed to help them return to baseline.
Young Stroke: A Program for All Ages
As therapists and clinicians, we know that the impact of a stroke extends well beyond the survivor’s physical deficits. Patients can be deeply impacted emotionally, socially, and financially, and the impact often ripples out to affect family, friends, and colleagues. The toll can be even more devastating if the stroke survivor was a significant financial contributor in their household, provided care for a young child or family member, or was pursuing education.
In 2010, Gaylord established its Young Stroke program, a segment of its inpatient stroke program, with the specific goal of preparing survivors who led active lives at the time of their stroke to return to as close as possible to their baseline level of activity through aggressive rehabilitation and a highly individualized, goal-driven plan of care.
The program’s name, “Young Stroke,” can be deceiving. Although more than 45% of Gaylord’s inpatient stroke population is 65 years old or younger, the primary qualification for the Young Stroke Program is not based on age. Rather, eligibility is directly related to the patient’s level of activity prior to their stroke, particularly if they were:
- Significantly and actively employed
- A student, or,
- A primary caregiver
Those with goals to return to any of these functions post-stroke—regardless of age—may be deemed good candidates for the program.
A Different Approach to Stroke Rehabilitation
The Young Stroke program takes advantage of the overall greater levels of energy and resiliency of this patient population. Stroke survivors who were very active prior to their stroke are often ready, willing, and able to participate in a more focused, rigorous program to help them return to the life they led pre-stroke.
Last year, 38% of Gaylord Specialty Healthcare’s inpatient stroke population participated in the “Young Stroke” program, their ages ranging from 15 to 82 years old, with the average age of 55. In comparison, the average age of stroke patients who did not fall into the Young Stroke program was 72.6, with ages ranging from 30 to 96.
The Young Stroke patient’s journey begins in the inpatient setting with a strong, interdisciplinary care team consisting of medical, nursing, therapy, care management, psychology, nutrition, respiratory, and chaplain services. Goal setting begins on day one and is considered the nucleus of the patient’s plan of care.
Most survivors participate in three hours of therapy per day or more, consisting of one-on-one and skilled group sessions with activities to promote fine motor coordination, cognitive skills, balance, and mobility. Survivors can also participate in activities with therapeutic recreation including cooking skills, virtual reality, visits with the therapy dog, and yoga. Survivors also participate in a stroke education series to learn about the anatomy of their stroke, recovery challenges, and advocacy.

Photo: Karen Ingham Photography
Skills to Return to Former Activities
In addition to participating in an aggressive physical, occupational, and speech therapy program, Young Stroke patients work on regaining or improving the particular skills they need to achieve their goals of returning to school, work, or caregiving.
When working with students in the Young Stroke program, speech and occupational therapists may be involved in finding adaptive techniques or equipment to help them take notes or exams. Therapists may also make recommendations to the school to ensure the student’s long-term success.
A survivor who is a primary caregiver may engage in activities related to caring for a child such as picking up an infant or toddler, feeding, diapering, bathing, dressing, or transferring the child to a car seat, crib, or stroller. To facilitate the transition to home, family training with the patient’s significant other is encouraged to help in sharing the care of the child and building the survivor’s confidence in handling skills required at home.
A survivor who was previously employed may practice his or her typing skills on a computer or work on tasks such as spreadsheets. If handwriting or the use of hand-held tools is central to performing a patient’s specific job, a therapist may work on grip strength and upper extremity strength with the help of robotics and electrical stimulation. Young Stroke patients also have access to a number of other technologies including a body-weight-supported gait and balance system to safely challenge a patient’s balance while walking. Consultations with a neuro optometrist to address any potential vision or attention deficits are also often incorporated into a patient’s plan of care.
Many survivors express their desire to return to driving. Before discharge, they are offered education on available return-to-driving programs and timeline expectations. When appropriate, they may participate in a brake reaction test to evaluate reaction time as one component of the gross motor skill of driving.
Young Stroke Program Discharge Plans
As their journey continues, the survivor will participate in discharge planning as the team works with them and their families to create a safe discharge plan. Last year, nearly 62% of Gaylord’s Young Stroke patients were discharged to home, either with or without home care services. In comparison, 41% of stroke patients who do not fall into the Young Stroke category were discharged to home. Many patients in both programs continue their recoveries with outpatient neurorehabilitation services.
A small segment (fewer than 5%) of the Young Stroke inpatient population is discharged directly to Gaylord’s on-campus Traurig House, the state’s only transitional living home for people recovering from brain injury and stroke. The residential program offers a home-like setting with programs to support daily living skills and access to the Gaylord outpatient rehabilitation they need to further regain the skills and confidence to successfully return to their homes and communities.
Case Study: College Professor
Andy*, a professor in his early 40s and father to young children, had a stroke that left him with severe speech and short-term memory deficits. Andy had two goals: to return to caring for his children and to return to the classroom the next semester.
After his inpatient stay, Andy was discharged to live in Gaylord’s Traurig House and continued with outpatient therapy through the hospital’s Day Treatment Program.
In addition to rigorous physical and occupational therapies, Andy worked closely with a speech therapist to help him meet his lofty goal of returning to teaching only six months later.
In an effort to make Andy’s therapy as realistic as possible, the speech therapist encouraged him to revise his syllabi for the upcoming semester to help him work on fine-tuning his language and memory strategies. The therapist also encouraged Andy to arrange and present a mini-lecture to scores of Gaylord employees during their lunch hour. For weeks, he worked on preparing a lecture to fit the allotted time, creating a visual presentation, and practicing his verbal skills.
The rigorous preparation and shot of confidence that his preparation and subsequent successful presentation gave Andy enabled him to fulfill his goal of returning the following semester and, most importantly, be active with his kids once again.
Case Study: Working Grandmother
At the age of 55, Dara* was employed full time and was actively involved in the life of her grandchild when she suffered a stroke in the right posterior basal ganglia region of the brain. Her goals were to go home, regain the use of her left side for an eventual return to work, and help out in the care of her grandchild.
She initially presented with a flaccid left side and worked tirelessly in her therapies to regain her independence. Dara was able to take advantage of many of Gaylord’s technologies to assist in her recovery, including an e-stim device for her upper extremity to assist with hand function and lower extremity to assist with foot drop, an overhead body-weight support system to challenge her balance and gait, and a bionic exoskeleton to gain endurance and confidence with weight bearing.
Her initial falls risk as measured by the BERG balance scale was a 6, indicating a high falls risk. At discharge, Dara scored a 42 on the BERG, indicating a low falls risk.
She initially required 75% assist of caregiver for upper body dressing, 100% assist for lower body dressing, and 25% assist for toileting. Upon discharge directly to home, Dara was independent for toileting and dressing and required supervision for showering.
Dara’s initial Fugl Meyer Score (a measure of upper extremity function) was a 16 for her left upper extremity and upon discharge she scored a 25/66 for her left upper extremity, indicating that she had gained mobility in her shoulder, elbow, wrist, and hand function. Within an inpatient length of stay of three weeks, Dara went from a 25% assist for mobility to supervision to modified independent level at home with continued therapy.
Dara was recently discharged home with the recommendation of continued therapy through Gaylord outpatient.
Both case studies are excellent examples of how Gaylord’s Young Stroke program drives exceptional outcomes.
In conclusion, survivors of any age who led active lives at the time of their stroke can greatly benefit from such an inpatient program to prepare them to return as close as possible to their baseline level of activity through aggressive rehabilitation and a highly individualized, goal-driven, and interdisciplinary plan of care.
*Name changed.
Stephanie Zanvettor, PT, CBIS, CCI is an inpatient physical therapist for Gaylord Specialty Healthcare in Wallingford, Conn. She received her master’s degree in physical therapy at Ohio University and currently specializes in neurological rehabilitation and has a passion for working with patients after stroke and traumatic brain injuries.
Main Photo Caption: Stroke survivors who were very active prior to their stroke are often ready, willing, and able to participate in a more focused, rigorous program to help them return to the life they led pre-stroke. Here, a patient practices cooking skills. Photo: Karen Ingham Photography
References
1. Stroke Facts. Centers for Disease Control and Prevention. https://www.cdc.gov/stroke/facts.htm
2. U.S. Stroke Rate Declining in Adults 75 and Older, Yet Rising in Adults 49 and Younger. The American Stroke Association. Feb. 3, 2022. https://newsroom.heart.org/news/u-s-stroke-rate-declining-in-adults-75-and-older-yet-rising-in-adults-49-and-younger