An accessible aquatic environment can benefit post-stroke and spinal cord-injured populations by facilitating a variety of activities in a safe, comfortable environment.
by Elizabeth Louie, CTRS
Community-based water exercise programs and aquatic therapy programs are on the rise. Physicians, clinicians, patients, and community participants agree that exercise and movement in water is often easier, safer, and more comfortable than on land. Buoyancy properties of water offer low impact, less joint stress, and lower risk of falling while enabling resistance, building of strength, cardiovascular fitness, and a general feeling of accomplishment and confidence with participation.
In the “early days” of aquatic therapy programs, they were oftentimes delivered in indoor community multiuse pool facility settings, such as YMCAs, gyms, or hotel pools. These types of facilities would offer to partner with agencies or provide rental space to organizations that wanted to offer water-based therapeutic activities, but lacked their own pools. In these settings water temperatures frequently were found at between 84 and 86 degrees, while additional activities such as swimming lessons, swim team practices, or water aerobics were being conducted in the same space.
Conducting therapy in a shared space with recreational swimmers or families enjoying leisure swimming could often invite challenges, such as maneuvering in an environment that could become crowded, and where high levels of noise and splashing might easily distract a patient’s attention away from therapy sessions. Another challenge created by a shared-space pool is scheduling conflicts. Therapists and aquatic therapy programs require pool use on a flexible schedule, and oftentimes patient care might need to be delivered in the evening, with rotations of physical therapist (PT), occupational therapist (OT), and therapeutic recreation (TR) therapists each having a patient. Providing therapy in off-site locations meant that some patients and therapists would require transportation between an inpatient facility and the pool location by either van or private transportation agency. For rehabilitation providers such as Kessler Institute for Rehabilitation, the payoff of establishing an in-house pool facility was clear: It would help reduce schedule conflicts and workplace distractions. Therapists and patients would be able to work in a setting with significantly improved access, free from the noise and crowding of leisure swimmers.
A Setting for Function and Focus
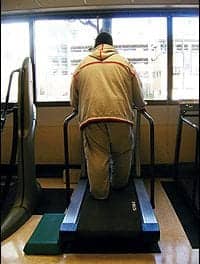
Kessler Institute for Rehabilitation (KIR), Marlton, NJ, Campus, provides water-based therapy services that are delivered in a focused, professional surrounding. These services are delivered in a therapeutic pool with water temperatures that are set between 92 and 94 degrees, and an ADA-approved lift provides entry and exit from the water for individuals who have mobility impairments. The lift operates from a fixed position, is water powered, and has flip-up arm and foot rests. It also features a seatbelt to enhance user safety, and is weight tested to 400 pounds. The pool is also built with steps that extend from the pool deck down into the water to a depth of 3 feet. In addition, two “baby steps” are placed between shallow and deep water that are helpful for beginners. Adding to this pool’s rehab functionality is a set of parallel bars installed in a section with 3-foot water depth and a section that is 4½ feet deep. A bench seat with jacuzzi jets directed at it is also installed in the pool.
Available for inpatient, outpatient, and aftercare participants, appropriate diagnoses for consideration include brain injury (BI), stroke, orthopedics, spinal cord injury (SCI), pain management, amputee, and multiple sclerosis (MS). For people affected by MS, a water temperature in the mid-80s is recommended. However, some members of that patient population tolerate or prefer warm water. Contraindications to any therapeutic activities in the aquatic environment can include open wounds/tubes/bracing and incontinence. However, several incontinence undergarments specific to aquatic use can be used as needed. Additional contraindications include behavioral inconsistencies, seizure, unstable blood pressure (BP), or unstable blood sugar. Aquatic therapy is prescribed by physician order, provided by licensed and certified clinicians, and is usually covered by insurance or included as part of a comprehensive acute care inpatient rehabilitation program.
Getting Started with Water-Based Therapy
The clinical advantages of therapeutic activity conducted in a water-based environment may not always be initially clear to patients and their families or caregivers. Patients and families are often introduced to the concept or use of aquatics at KIR, Marlton Campus, by the hospital liaisons in the acute care setting. Upon inpatient admission, one-on-one or co-therapy sessions can be initiated by MD, PT, OT, or TR, often based on admitting diagnosis, or requested by the patient or family after initial evaluations. An overview and tour of the pool area are provided, and the patient’s previous comfort levels for aquatics are investigated.
It is essential for every aspect of aquatic therapy to be practiced with utmost safety. One of the safeguards in place at this Kessler facility is for all inpatient sessions to have staff in the pool. (The author is currently American Red Cross Lifeguard certified and previously adapted aquatics and WSI certified.) Likewise, all OP staff have ARC Basic Water Safety Certification. The initial session is typically conducted as a co-therapy by a combination of PT, OT, or TR therapists, with a duration of 45 minutes or 90 minutes. Also, during the initial session, basic safety and goal(s) are discussed with therapists who provide input about how transfers are to be conducted and the type of therapeutic exercise that will be performed. Likewise, standing and mobility are discussed in addition to discussion that promotes use of aquatic properties, stroke mechanics, games, activities, and “props” (ie, aquatic equipment). The patient is also given the responsibility of alerting the therapist about adverse reactions during the session, such as pain or dizziness.
An accessible aquatic environment can benefit the post-stroke and SCI populations by offering choice of hobby (premorbid or newly developed) and inclusion with family/friends/like-minded peers (member or group) in a therapy/exercise/wellness environment. Entry and exit from the pool via steps transitions can be supported by land-based learning, such as addressing the question of, “Which leg goes first?” It also offers the opportunity to reinforce safety and memory for techniques such as moving forward or backward, use of handrails, set over step, and level of assistance needed. Use of a pool lift can help carry over strategies for practicing wheelchair transfers while enabling the therapist and patient to reinforce safety concepts and practice techniques for change of direction and slide board.
Pool Accessories for Versatile Activity
Patients/participants can maximize functional movement ROM and strengthening; directing care for PROM, AAROM, or modified swim strokes, types of therapeutic exercise, investigating stroke mechanics, breath control, and endurance. Positional changes can offer opportunity for supported/modified weight bearing and ambulation/step training using ankle/wrist weights to increase joint/body proprioception, balance, and resistance in parallel bars or along the wall. Extended vertical or horizontal stretching using floatation belt, Coast Guard-approved life jacket, or noodles offer a sense of relaxation or freedom. Additional goal areas and use of “props” in aquatic sessions include: enhancing sitting balance using a balance board, forward leaning over a kickboard and right/left trunk twist sitting on the bench seat, pain/stress management using the jacuzzi jets or noodle-supported floatation, cognition/communication with use of aquatic terms, recall of previous sessions, family education/support/resource awareness with creation of National/community Diagnosis organization relationships, and community health/wellness facilities/programs, student education for practical “hand’s on” experience, and potential case study.
Activity Parameters
Aquatic therapy frequency typically is 1 to 3 days per week and depends on benefit from and tolerance of a trial session, the patient’s medical stability, and the patient’s own attitude toward therapy. For therapy to succeed, there must also be an ongoing agreement about scheduling for the therapist and patient. Schedules are often planned so that following OT sessions can carry over to showering and dressing goals; these often may be done in the locker room, which simulates a “community locker room” setting.
Upon discharge, many patients will return to KIR, Marlton, outpatient clinic. Land-based PT can be enhanced by aquatic PT—a therapy plan of care is developed upon initial evaluation and interest/previous participation in aquatics is discussed. Sessions may be reduced based on overall frequency of outpatient therapy, or can be increased based on medical need (ie, weight bearing status, pain management). Resources for community-based programs or aftercare programs may be discussed, and therapists will transition patients by offering observation of the aftercare program and introduction to this certified therapeutic recreation specialist, who is the facilitator.
Available following discharge from all skilled therapy, KIR—Marlton offers an Aftercare Aquatics Program. Offered up to 3 days a week, it is offered as a fee-for-service program (eight complimentary tickets are given upon completion of outpatient therapy) and designed to enhance mobility, ROM, posture, balance, endurance and socialization. Participants may bring a companion to assist as needed for this program, which has been growing since becoming part of the Kessler family in 2016.
Jumping In Feet First
Finding and participating in the right aquatic program can be daunting, but proactive and positive feedback from participants and staff can make the idea and opportunity more comfortable. For rehab directors or facility managers weighing the possibility of bringing aquatic therapy in-house, the best way to inform that decision may be to look for resources and connections in the local community; to ask questions and observe, and ultimately to try it! A helpful mind-set is to be open to “new” things that have yet been untried. Once aquatic therapy is put into operation, the combination of treatment strategies that usually are most successful over the long term include exercise, medication, therapy, social support, and lifestyle modification. Creating and adjusting to programs takes time, and new trends such as Aqua Zumba, Ai (Tai) Chi, and paddleboard yoga are always on the horizon. Effective therapy can be delivered without knowing how to swim or getting one’s hair wet, which means the key to success may boil down simply to the willingness to get in feet first! RM
Elizabeth Louie, CTRS, is a recreation therapist with 32 years of experience in physical medicine and rehabilitation, and aquatics. For the past 2 years she has worked at Kessler Institute for Rehabilitation—Marlton Campus, where her responsibilities include assessment and treatment for adults affected by varying diagnoses that include SCI, orthopedic conditions, amputation, MS, BI, stroke, and other neurological conditions. Louie is a member of the Stroke Committee, facilitates inpatient activities, stroke education, one-on-one and co-therapy, aquatic sessions, monthly community stroke support group, and Kessler’s Aftercare Aquatics program. Louie has a bachelor of science in recreation & parks management with a concentration in therapeutic recreation from West Virginia University in Morgantown, WV. For more information, contact [email protected].