Pressure ulcer or sore prevention and reduction have been a key focus of Healthy People 2010 and Joint Commission on Accreditation of Healthcare Organization and their long-term care national safety goals for 2007. In addition, a combination of the high cost to heal pressure ulcers, as well as the cost of litigation in cases where treatment has been below the community standard of care, has resulted in risk managers and administrators paying closer attention to pressure ulcer prevalence rates. Practice guidelines for prevention of pressure ulcers have been supported by clinical research and expert opinion. Little, however, has been published with regard to the disabled population—those of advancing age with disabilities such as cerebral palsy, muscular dystrophy, spina bifida, multiple sclerosis, and spinal cord injury. The purpose of this article is to bring into focus and share the lessons and experiences of preventing pressure sores and ulcers at Pennsylvania-based Good Shepherd Rehabilitation Network’s long-term care home for people with disabilities.
 |
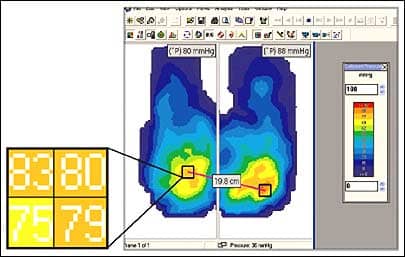
| Pressure mapping technologically charts surface changes as client weight is applied. |
PRESSURE ULCERS AND AGE OF PATIENTS
While pressure ulcers can and do occur at any age, risk increases with aging. Changes in the skin with advanced age include thinning and flattening of the epidermis, decreased epidermal turnover, a decrease in sensory perception, vascular fragility, a loss of subcutaneous fat, and decreased oil production. Therefore, aging skin is prone to skin tears and delayed wound healing.
The most common areas for the development of pressure sores in patients who are bed-ridden or confined to a wheelchair include the sacrum, heels, back of head, trochanter, ankles, and shoulders—anywhere there is a bony protuberance. Given the demographic of Good Shepherd’s permanent residents with disabilities, changes in bony structures such as contractures and curvature of the spine are common. This often limits turning surfaces, and ulcers sometimes occur in areas not seen in the general population. In these cases, staff uses positioning devices such as foam wedges, bolsters, and gel pads.
There are several myths regarding pressure ulcer prevention, and it is important to address and dispel them. Some of the more common myths are:
- Massaging red areas over bony prominences helps prevent pressure ulcers;
- You do not have to turn patients or residents over if they are on a special mattress;
- Egg crate foam overlays help prevent ulcers;
- Bunny boots or sheepskin relieves pressure on the heels.
CAUSES OF ULCERS
Ulcers are primarily caused by prolonged pressure over a bony prominence. The effect of the pressure on soft tissue is dependent on the intensity of the pressure, the duration of the pressure, and the tissue tolerance to the pressure. Other contributory factors include decreased activity, immobility, shear, friction, moisture, decreased sensation, and malnutrition. Increased risk for the development of ulcers can result from lack of sensation or feeling when, for example, a person suffers a stroke and is paralyzed on one side of their body. Another example is a person’s impaired ability to communicate pain. Comorbid conditions such as diabetes, impaired respiratory status, cardiovascular disease, renal disease, and other acute or chronic conditions also increase the risk of pressure ulcers forming.
Stress has been associated with increased risk of pressure ulcer development. Psychosocial status, including motivation and emotional energy demands, needs to be considered in a comprehensive prevention program. Meeting the resident’s psychosocial needs decreases stress. At Good Shepherd, visitors, family members, volunteers, clergy, and staff are encouraged to keep residents fully engaged by exposing them to music, movies, art, and meaningful current events.
ULCER PREVENTION FOR WHEELCHAIR-BOUND
Preventing pressure ulcers among permanent residents at a long-term care facility for the severely disabled is a challenge given that all residents are wheelchair bound. Good Shepherd is somewhat unique in that very few long-term care facilities have as diverse a population where residents have several different mobility-restricting conditions, such as cerebral palsy, spinal cord injuries, multiple sclerosis, muscular dystrophy, and spina bifida. Some of the residents arrived at the center as children more than 40 years ago.
 |
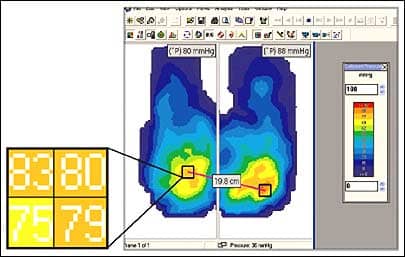
| Shirl Erb, PT (right), a therapist at Good Shepherd Rehabilitation Network, Allentown, Pa, uses pressure mapping software as part of Jennette Gigler’s treatment. Gigler is a long-term resident of the Good Shepherd’s Raker Center. |
The approach taken by Good Shepherd in the care it applies to its long-term residents is one of a village. Each member of the rehabilitation team focuses on making a positive difference in pressure sore prevention. Every single person who cares for residents is equally important to the caring process. Each resident is unique and receives an individualized plan of care.
Long-term care residents present a host of unique needs, and for this reason, pressure ulcer prevention needs to be an individualized, collaborative rehabilitation program. Often we think of nurses, physicians, dieticians, and physical therapists as members of a wound care team. However, the value and inclusion of social services, speech therapists, respiratory therapists, recreational therapists, as well as the residents in the prevention and treatment process better meets the needs of residents.
The assessment of our residents includes the use of the Braden Risk Assessment technique for risk prediction, and, based on these findings, we implement specific individual interventions to limit the risk of ulcers. A combination of new technology—such as pressure mapping—and clinical expertise for wheelchair seating is often used to meet a challenging resident body contour. Dedicated staff members attend to residents’ needs by routinely turning, repositioning, toileting, and observing the skin.
The value of speech therapy cannot be overestimated. About 60% of adults with cerebral palsy have speech or communications challenges, and communications issues also coexist with other conditions. The ability to communicate pain and the need to use the bathroom are very important in preventing pressure ulcers. Occupational and speech therapists are increasingly using assistive technology to improve patient communication, which, in turn, has a positive impact on pressure ulcer prevention.
On the rare occasions when residents are on bed rest and confined for more than 8 hours, a written turning sheet is employed and the need to implement the introduction of special mattresses and adjust the frequency of turning and repositioning is constantly reevaluated.
TREATMENT OF ULCERS
In the event that pressure ulcers do occur, it is extremely important to have a uniform approach that acknowledges there are no small wounds—every wound, even a scratch, must be taken seriously. The next step in the process is to understand how the ulcer happened in order to identify the cause. This is followed by a careful evaluation of the clinical and environmental information we need to implement a plan of care. This includes evaluating any recent illness the resident may have had, whether there has been recent weight loss, any histories of a previous ulcer, an evaluation of wound and related pain, and the resident’s behavior and/or refusal of care. All equipment used by the resident is evaluated and inspected by the wound team, including their mattress and wheelchair cushions.
All this information is captured in a wound assessment report, and ongoing comparisons are updated on a weekly basis. At this time, the wound care team determines the wound’s progress against the goals identified when the ulcer first occurred. Based on this information, recommendations are made to continue current treatment or to change direction. The primary physician sees the resident weekly and is notified of any changes in the ulcer’s status. The resident is kept informed of the wound assessment status as well as the wound care plan. Education is given and documented on wound rounds.
The role of family members cannot be overemphasized. They play a vital role in keeping their loved one engaged and an active participant in his or her surroundings. It is vital to include the family in all phases of care, including pressure sore prevention, by communicating with them, listening to them, and educating them on what they can do to make a positive difference. Family members are, in fact, encouraged to play an active role in the treatment process.
Taking a look ahead, we are already seeing an aging population in both the general and disabled population. People are living longer—even with chronic diseases. As better treatment, management, and, hopefully, even elimination of some of these chronic diseases advance, there will be a positive effect on the incidence of pressure ulcer development.
Additionally, given the rate of growth in both evidence-based research and medical technology, one can expect that someday we may have the potential to understand pressure ulcers and take preventive measures before they occur. For example, we may be able to identify risk at a cellular level and intervene prior to the occurrence of tissue injury. One thing is for certain, education and caring will remain as important in the future as they are today, and those who provide care will always be the best defense against pressure ulcer development.
Nancy Martucci, RN, BSN, CWOCN, is a certified wound, ostomy, and continence nurse in the occupational therapy department, Good Shepherd Rehabilitation Network, Allentown, Pa. For more information, contact .