 |
SOURCES
|
When bariatric specialist Michael Dionne, PT, first treated a patient who weighed more than 1,000 pounds, he had to improvise. The year was 1985, and devices made specifically for bariatric patients were practically unheard of.
In the absence of a bariatric standing frame, for example, Dionne fashioned his own by bolting a bed to a wall frame. “In the old days, there was no equipment,” says Dionne, owner of Choice Physical Therapy (www.bariatricrehab.com), Gainesville, Ga. “We made it up.”
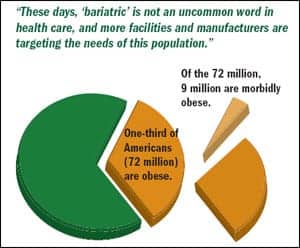
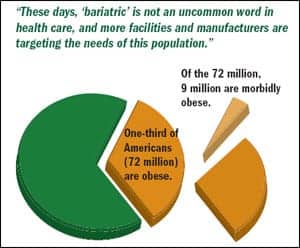
These days, “bariatric” is not an uncommon word in health care, and more facilities and manufacturers are targeting the needs of this population. Approximately one-third of American adults—72 million people—are obese.1 Of these, 9 million are considered morbidly obese, meaning that they are more than 100 pounds overweight or their body-mass index (BMI) is greater than 40.2
The prevalence of obesity has created a demand for hos pitals and health care providers to accommodate these patients. Some facilities are even building bariatric suites. “Every hospital, regardless of whether they’re engaged in the treatment of obesity, is beginning to look at meeting the basic needs of a bariatric patient,” says Kevin Huffman, DO, founder and president of American Bariatric Consultants, Cleveland, and consultant for Gendron, Bryan, Ohio.
Cost is a predominant challenge to overcome when planning care for bariatric patients. Prolonged length of stay combined with Medicare cuts often discourages administrators from investing in the needed equipment and personnel. However, having the right tools in place improves the safety and efficiency of care—which ultimately benefits the bottom line. “Our job is really to help transition a patient through the continuum of health care in a cost-effective manner,” Dionne says. “Incorporating equipment sooner will make things more cost-effective in the long run.”
ENSURING SAFE TRANSFERS
Working with bariatric patients, who present with a variety of complications, requires OTs and PTs to use their entire skill set.
“I can’t think of any patient population that presents with greater weakness relative to body mass,” Dionne says. “This patient population challenges the therapist to draw upon everything they’ve ever done with every type of patient. So, you draw on outpatient orthopedics, you draw on your cardiopulmonary, and you draw on your psych/social.”
 |
A transfer—from a bed to a wheelchair, for example—is one of the most precarious situations for both bariatric patients and their health care providers. The risk of injury is high, especially if the proper precautions are not in place, and this can translate to high costs for the health care system.
“We’ve seen studies that an injury to a health care provider can cost a hospital up to $50,000, because you not only have that injured health care worker who now needs health care themselves, but also they’re on disability payments, there are workers’ comp claims against the hospital, and the hospital has to hire a new person and train a new person,” Huffman says. “So, it’s very costly.”
It is no wonder, then, that legislators are working toward “no-lift” policies to reduce the number of back, neck, and other related injuries to health care providers. But no matter how you handle a patient transfer, avoiding injury requires a systematic approach.
“You just can’t go in and say, let’s go lift this patient,” Huffman says. “The OT or PT has got to stop and say, what size is this patient, how much does this patient weigh, and what’s our capacity on this equipment? Because ultimately, if they get injured or the patient gets injured, the OT or PT will be taking responsibility.”
Before mobilizing a bariatric patient, for example, it is important to assess the patient’s mass distribution, as Dionne notes in his book, Among Giants: Courageous Stories of Those Who Are Obese and Those Who Care for Them (Lulu.com, 2006).
“The idea is that you can predict mobility patterns in a sizable patient based on their mass distribution,” he says, adding that failure to predict these patterns can lead to breathing difficulties and other complications. “You have to understand there’s greater diversity in the population of size—there’s more to it than apple versus pear.”
 |
These assessments also influence what types of transfers are required. For example, transferring a 500-pound patient who is 4 feet, 11 inches tall to a wheelchair for therapy may be a safer, more effective choice than using the bed. “There’s no bed in this world that goes low enough for that patient, especially if they have pear-shaped distribution,” Dionne says.
You also need to have a lift team in place. PTs and OTs play a central role in developing a lift team as well as setting policies on how to transfer bariatric patients safely. According to Huffman, this team usually includes PTs, OTs, nursing staff, and even discharge planners.
Injuries occur when health care providers make hasty decisions to lift without the proper support staff or equipment. Staffing shortages or budget constraints are common challenges to overcome, but investing in equipment and personnel can save hospitals the much higher cost of injury. “The PTs and OTs have to engage the administration to make sure that proper lifting techniques are developed and implemented, that the lifting team is in place, and that proper equipment, where it’s available, is utilized,” Huffman says.
The right equipment is key to a successful transfer. According to Dionne, there are three main pieces of equipment required for bariatric care: a bed, a lift, and a wheelchair. This bariatric triad, as he calls it, is ideally portable so that the equipment can be used in any wing of the hospital.
A bariatric bed should be weight-rated with an expandable support surface. Some beds can also be lowered to within 6 inches of the floor, allowing some types of treatment to take place without a transfer. “The bed is the rehab platform, so it’s where everything starts,” Dionne says.
Dionne has a high regard for ceiling lifts and recommends that they be installed over every bed in a bariatric suite, when it is feasible. But he notes that hospitals cannot always afford this option and that the lack of portability can be a serious drawback, as it limits care to the bariatric suite alone. “I like the bedside lift as an option because it can pick up patients who fall in the hall or in the parking lot, where a ceiling lift isn’t going to work,” Dionne says. “And the bedside lift can follow the patient as the patient transitions through the continuum of health care.”
He recommends a sling-loading bedside lift with at least a 750-pound capacity that allows you to move the patient from supine to supine, to transfer from the wheelchair to the bed, and even to lift from the floor. Lifts are also available to rent, which can be an affordable solution for hospitals that use them only rarely.
Bariatric wheelchairs should have a 750-pound capacity with at least a 34-inch width. Footrests should move easily out of the way for smoother transfers. Some hospitals may be tempted to skip this item because of cost, but Huffman cautions against this line of thinking. “They’ll say these bariatric wheelchairs are just too expensive, we’re not going to get them,” Huffman says. “Well, one injury to a patient or one injury to a health care provider would have paid for a dozen of those wheelchairs.”
Make sure to invest in quality products that can withstand the weight of the patient. “When you’re looking at equipment, you’ve got to look at how well it’s built, what is the lift capacity of that portable equipment, and how it’s designed,” Huffman says. He cautions that some products may advertise the correct capacity but may not be wide enough or stable enough for the patient.
OUTFITTING THE HOME
When patients transition to the home, Huffman advises PTs and OTs to make sure they have the same types of equipment that they used in the hospital. This means ensuring the same bariatric triad is in place—which often isn’t the case.
 |
“I used to go out and see my patients in the homes because they just weren’t able to get out,” Huffman says. “I’d see patients sleeping on the floor, or I’d see them sleeping in a recliner. That’s just not dignified, nor is it safe.”
Ask patients to describe their home and the equipment they already have. Find out what their sleeping arrangements are, and make sure to recommend a bariatric-rated bed. Also, discuss the distance from the bedroom to the bathroom. As incontinence is a common complication for bariatric patients, a bedside commode is often a necessity. In the bathroom, a bedside commode can also be placed over a traditional wall-mounted toilet, which cannot support a bariatric patient.
There are other items to consider as well, such as shower chairs, grab bars, and hand rails. “We want to give them some sense of independence and certainly some dignity,” Huffman says. “They would prefer that they take care of some of these hygiene issues, if we could provide that equipment.”
Due to lack of movement and moisture buildup, skin breakdown is a common problem for bariatric patients, particularly in the heels, elbows, and lower back. This is important to keep in mind when choosing a mattress. “You need a surface that has very little friction associated with it and that retards fluids so that the fluids will run off of it,” Huffman says.
Specially designed bariatric mattresses with alternating air pressures are available to help prevent decubitus ulcers. However, Medicare will reimburse for this type of mattress only if the patient already has skin breakdown. Huffman hopes that this will change, as preventing decubitus ulcers, which can last for months or even years, is much less painful for the patient and will ultimately cost less to the health care system.
ASSESSING TOTAL HEALTH
The best way to keep up with trends and best practices in bariatric care is to attend seminars at national conferences, such as those put on by the American Society for Bariatric Physicians and the American Society for Metabolic and Bariatric Surgery. Some manufacturers also sponsor continuing-education seminars, such as those Huffman delivers for Gendron.
In addition to the clinical knowledge required, sensitivity is key when working with bariatric patients. “Put yourself in their place, how embarrassing it is. These patients don’t want to be this size,” Huffman says. “Do everything you can to make them feel comfortable, and let them know that you are empathetic to their position.”
Becoming an advocate for these patients also gives therapists the opportunity to assess their total health. Many bariatric patients are actually malnourished, and they require nutritional support to maximize the effectiveness of rehabilitation therapy. “Some of their diets are higher in refined carbohydrates, and you’ll find deficiencies and B12 deficiencies,” Huffman says.
In some cases, the PT or OT is the first point of contact the patient has had with a health care provider in years. Encourage patients to resume their regular screenings, such as mammograms, PAP smears, and prostate exams. “What we’re finding is that these patients have much higher risk of dying of cancers,” Huffman says. “Part of that is due to the obesity, but part of it is because they’re lacking screening because they are not getting in the health care system.”
Ultimately, working with bariatric patients can be rewarding. “For the therapist, there is no greater fun than to see a patient achieve success over adversity, and here you’ve got plenty of challenges,” Dionne says. “It’s just getting the coordinated team to be able to do it in a manner that’s safe.”
REFERENCES
- Ogden CL, Carroll MD, McDowell MA, Flegal KM. Obesity among adults in the United States—no statistically significant change since 2003-2004. Division of Health and Nutrition Examination Surveys. Available at: www.cdc.gov/nchs/data/databriefs/db01.pdf. Accessed September 25, 2008.
- All about obesity. Obesity Action Committee. Available at: [removed]www.obesityaction.org/aboutobesity/morbidobesity/mo.php[/removed]. Accessed September 25, 2008.