Vestibular testing alongside balance and gait dysfunction evaluation sets the stage for optimal treatment in older adults.
by Beth Kauffman, MPT, ATC

VISION
It is well documented that visual changes occur with aging, whether it is macular degeneration, glaucoma, or the need for bi-focal lenses. The medical community has treatment options for these pathologies to minimize visual deficits and optimize function of the visual system. Vision therapy is a treatment option available for retraining focal deficits. Additionally, physical therapists should utilize a comprehensive treatment approach that includes gaze stabilization exercises, particularly in older adults with complaints of dizziness. Dizziness is a frequent complaint of this population, which causes falls and affects gait stability and balance.
SOMATOSENSORY
Somatosensory changes also occur with the aging adult for various reasons. There are documented changes of neuromuscular function as we age, including decreased motor unit recruitment, nerve conduction velocity, and cross section of muscle fibers. These and other changes affect the somatosensory input, which is one component of having normal walking abilities. Many persons with gait and balance dysfunction present with lower extremity pathology that has caused physiological changes in the body. These changes affect sensory input at the ankles and result in improper neuromuscular control and decreased or abnormal balance strategies. A range of approaches can be used to assess these strategies, including the integration of pressure mapping to capture sequential footsteps for analysis of foot function and gait, and to provide automated calculations of a variety of gait parameters. Frequently, a larger velocity movement is utilized as a result of deficits with smaller velocity ankle strategies to maintain balance. This may include a hip/trunk or stepping strategy. Global body muscular weakness and lower extremity loss of joint range of motion also may be contributing factors to deficits in the somatosensory system, and may be assessed through the use of force plates to aid in the design of effective treatment and/or training programs for patients that center on these specific sensory and motor components.
ADDITIONAL BALANCE TECHNOLOGIES
A variety of treadmills also can serve as key components in skilled physical therapy intervention for the debilitated patient. Gait retraining and balance improvement can be facilitated using a full body weight supported (BWS) treadmill system or partial body weight supported treadmill (PBWST). Gait trainer treadmills offer features that can measure cadence, step length, step width, speed, and incline to provide therapists the means to make gross and fine-tuned adjustments during gait training.
VESTIBULAR
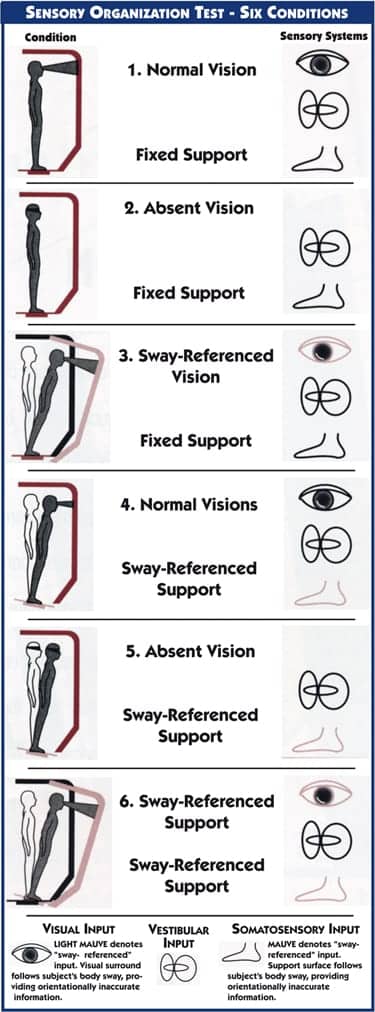
The third system that promotes balance and stability is the vestibular system, which is well known for causing dizziness complaints that are frequently treated with medication, rest, or physical therapy. In older adults, the vestibular deficit is not as apparent, due to comorbidities and the complex integration of systems to maintain balance. It is important to isolate each system and how they work together during evaluations to guide treatment. The vestibular system is objectively evaluated using a balance management device. There are many tests available on this type of system to treat and assess vestibular and balance dysfunctions. One specific test, the Sensory Organization Test (SOT), assesses the visual, somatosensory, and vestibular systems and their integration with each other to maintain static balance. There are six conditions to the test, which can be seen in the diagram in this article.
Research presented at the Gerontological Society of America Scientific Meeting 2011, titled “The role of the vestibular system in gait and balance dysfunction,” utilized a specific type of balance management system to determine deficits in the visual, somatosensory, and vestibular systems in older adults. The SOT was completed with these subjects, who all had a chief complaint of gait abnormality or balance problems. Three categories were used, separating the subjects by age: 61 to 74, 75 to 84, and more than 85 years. The results indicated that abnormal vestibular function was present in all three categories.
Vestibular system deficit is one component of balance and gait dysfunction. Dizziness is a common patient complaint that may indicate vestibular dysfunction is present. However, dizziness also may be attributed to medication side effects, orthostatic hypotension, central nervous system pathology, and various other reasons. The inefficiency of the vestibular system to process information results in loss of balance and increased fall risk. The vestibular system needs to communicate with both the spinal and visual systems to respond to balance challenges and maintain stability. The integration of a body weight support system also may be used to clear the line of communication between these systems, allowing for the creation of an environment that offers customized support and adaptability for patients with varying levels of debility, while also preventing falls.
Retraining of the vestibulo-oculo reflex (VOR) is well documented in the rehabilitation literature through specific exercises. However, this is not commonly thought of as a treatment approach for rehabilitation of older adults with gait and balance dysfunction. After a thorough PT evaluation, it is important to prescribe a few simple exercises at home, then progressively challenge the VOR in static and dynamic environments in the clinic. These exercises require close observation of eye movement and guarding at all times due to the possibility of loss of balance. VOR exercises easily integrate into skilled physical therapy intervention with the goals of improving gait, balance, and decreasing risk for falls. This may include VOR activities that challenge balance on uneven surfaces or while walking. Additional progressions include going from a plain or quiet background to busy surroundings. (article continues below)
PRACTICAL CLINICAL TESTS FOR EVALUTAION OF VESTIBULAR DYSFUNCTION
There are many other field tests that can be done if no balance management system is available. Several examples follow:
Gait Speed: A 10-meter gait path can easily be done to assess someone’s velocity. Norms for age and gender have been well documented in the literature.
The Dynamic Gait Index is an eight-item assessment tool used to evaluate gait at different speeds, with head movement, while stepping over or around obstacles and on stairs. A score of < 19 out of 24 indicates increased risk for falls in community-dwelling older adults. The first four conditions are mostly vestibular specific. Marchetti et al have reported a score eight out of 12 for the first four conditions indicating increased risk for falls.
Romberg Testing on level and unlevel surface. Be sure to indicate stability as minimal, moderate, or severe sway, or fall. The goal is to hold the position for 30 seconds.
Dynamic Visual Acuity Testing: Using an ETDRS Chart at 2 meters, have the patient turn their head with eyes focused on the lowest clear line at 2 Hz (240 bpm, one click for each directional head turn) until unable to focus on the original line. A two- to three-line change is significant, indicating a slippage of the image on the retina and VOR dysfunction.
Head Thrust Test: Indicates VOR dysfunction. Look for a “catch up” movement of the eye during a tester-induced rapid head turn while the patient focuses on a target.
AGING TOPICS THAT AFFECT VESTIBULAR FUNCTION
Other than general vestibular system decline and changes in reflexes, older adults frequently present with loss of cervical range of motion as part of the vertebral spine degenerative process of aging. With changes or loss of cervical range of motion, less stimulation is occurring to the vestibular system, which may contribute to faulty balance mechanisms and changes in feedback through the VOR.
In the research noted above completed by Kauffman et al, there was a trend noted of women having greater vestibular dysfunction as compared to men. It is noted as only a trend as it did not meet a 0.05 level of statistical significance with a chi square test. However, it may be inferred that women are more likely to have vestibular dysfunction due to osteoporotic changes in the boney structure of the inner ear.
CONCLUDING REMARKS
Incorporating vestibular testing into balance and gait dysfunction evaluation is essential for optimal treatment of the older adult patient. Our current trend is noting a significant increase in vestibular and visual scores on the SOT after a course of 4 to 6 weeks of outpatient balance and gait physical therapy. Regaining and improving balance greatly increases a person’s confidence and quality of life. We look forward to completion of further research to statistically analyze outcomes before and after physical therapy intervention. RM
Beth Kauffman, MPT, ATC, is a private practice physical therapist and certified athletic trainer at Kauffman Physical Therapy in Lancaster, Pa. She treats a broad adult orthopedic population and older adults with problems related to gait, balance, and falls. Kauffman’s continuing education includes many national and international physical therapy conferences and contribution to the upcoming third edition of the Geriatric Rehabilitation Manual to be published in 2013. For more information, contact [email protected]
REFERENCES:
Kauffman T, Barr J, Moran M. The Geriatric Rehabilitation Manual. 2nd ed. Philadelphia: Churchill Livingstone/Elsevier; 2007.
Hall C, Heusel-Gillig L, Tusa R, et al. Efficacy of gaze stability exercises in older adults with dizziness. J Neurol Phys Ther. 2010;34(2):64-69.