Recent study results indicate neurons derived from human induced pluripotent stem cells (iPSC) and grafted into rats post-spinal cord injury (SCI) produced cells with tens of thousands of axons, extending virtually the entire length of the animals’ central nervous system.
Scientists at the University of California, San Diego School of Medicine and Veteran’s Affairs San Diego Healthcare System, conducted the study, a recent UC San Diego news release states.
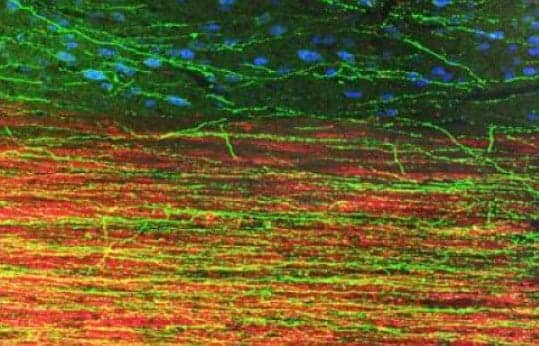
According to lead scientist Paul Lu, PhD, UC San Diego department of Neurosciences and colleagues, the human iPSC-derived axons extended through the white matter of the injury sites, frequently penetrating adjacent gray matter to form synapses with rat neurons. Similarly, rat motor axons pierced the human iPSC grafts to form their own synapses.
Mark Tuszynski, MD, PhD, professor of Neuroscience, director of the UC San Diego Center for Neural Repair, explains: “These findings indicate that intrinsic neuronal mechanisms readily overcome the barriers created by a spinal cord injury to extend many axons over very long distances, and that these capabilities persist even in neurons reprogrammed from very aged human cells.”
The current study reportedly builds on past research conducted by Tuszynski and colleagues, and earlier works have suggested grafted stem cells reprogrammed to become neurons can form new, functional circuits across an injury site, with the treated animals exhibiting some restored ability to move affected limbs.
In the current study, the release says, Lu, Tuszynski, and colleagues converted skin cells from a healthy man, aged 86 years old, into iPSCs. The release notes that the iPSCs were then reprogrammed to become neurons, in collaboration with the laboratory of Larry Goldstein, PhD, director of the UC San Diego Sanford Stem Cell Clinical Center. The new human neurons were subsequently embedded in a matrix containing growth factors and grafted into 2-week old SCIs in rats.
A total of 3 months later, the researchers say they investigated the post-transplantation injury sites. The researchers reportedly found biomarkers indicating the presence of mature neurons and extensive axonal growth across long distances in the rats’ spinal cords, even extending into the brain. The axons crossed wound tissues to penetrate and connect with existing rat neurons. Similarly, rat neurons extended axons into the grafted material and cells, the researchers state. The transplants also produced no detectable tumors, the release says.
Despite the numerous connections formed between the implanted human cells and rat cells, the release reports that no functional recovery was found. Lu notes in the release that the tests assessed the rats’ skilled use of the hand, however simpler examinations of leg movement may still show benefit.
Tuszynski adds that he and his team are working to pinpoint the most promising neural stem cell type for repairing SCIs, and are testing iPSCs, embryonic stem cell-derived cells and other stem cell types.
Photo Caption: This image depicts extension of human axons into host adult rat white matter and gray matter three months after spinal cord injury and transplantation of human induced pluripotent stem cell-derived neurons. Green fluorescent protein identifies human graft-derived axons, myelin (red) indicates host rat spinal cord white matter and blue marks host rat gray matter.
Photo Credit: UC San Diego School of Medicine
Source: University of California, San Diego