 |
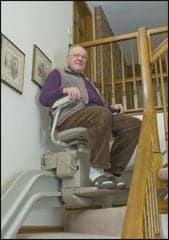
| Bill Noonan of Littleton, Colo, enjoys the accessibility his stair lift provides. Photography by Jeff Uhrlaub |
In the continuum of care for people who are recovering from serious injury, or for those who simply wish to age in place, living at home with independence and safety may seem like a mirage, like the impossible dream. If they have limited mobility, they may wonder: how will I mount steps by the front door, reheat coffee in the microwave, take a shower, or watch TV? Adapting accessible living space with Universal Design principles and modifications helps foster independence and mobility for people who choose to age in place or for those who have traumatic brain injury (TBI), spinal cord injury, and other disabilities. Solutions, both high and low tech, and in all price ranges, abound.
Individuals may be ambulatory or use a manual or a power wheelchair to get around, but during rehabilitation—even before they return home—preparations begin for adapting the home to accommodate their changed, and perhaps changing, abilities and skills. Occupational therapists make general and specific recommendations that can entail short- and long-term modifications to be adopted over time, as needs and funding permit. The priorities: establishing an entrance/exit in two separate areas of the home in case of emergencies, and making living spaces more user-friendly.
GROUND ZERO—DETERMINING NEEDS
Spinal cord injury patients often have sensory deficits, which impact sensation in different parts of the body. They may have impairment in the use of their hands, arms, trunk, or legs, and may have restricted mobility, whether getting around in bed or in a wheelchair, or sometimes in being able to walk, says Krista Mackenzie, OTR/L, Clinical Director of Inpatient Occupational Therapy at Casa Colina Centers for Rehabilitation, Pomona, Calif. For someone who has TBI, therapists must consider memory issues, poor insight, visual impairment and inability to know how impaired they are and what they can and cannot do by themselves, she says. “They might have trouble with their memory, initiating activities, or decreased sensation, and they have trouble wandering because they don’t necessarily know how impaired they are, and they get up and try to walk out by themselves or maneuver around the house when it’s not safe,” she says. These individuals may also have decreased balance, concentration, problem-solving, and safety issues.
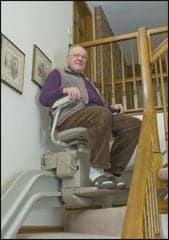
Clients with a higher-level spinal cord injury that limits physical ability, who need assistance through doors with side hinges, might benefit from technology-based compensation, such as automatic door openers and environmental control units. Individuals, such as wheelchair and scooter users, can open remote-controlled doors with ease-of-use with wheelchair-mounted controls, wall push pads, and any number of specialty controls that have been customized for almost any physical disability. For mobile patients who have use of their arms and hands, more physically based solutions may be key, enhancing access in halls, doorways, bathroom, bedroom, and kitchen, and perhaps adding railings on a ramp or staircase, to help avoid falls. For individuals who live in multilevel homes and have difficulty negotiating the stairs, an excellent solution to their dilemma is adding a battery-operated stair glide. Available in straight as well as custom-curved models, these devices offer users an easy solution to safely (and comfortably) access their entire home. For external access issues, vertical platform lifts can assist with access from ground to porch and deck levels, and are rugged enough for scooters and wheelchairs.
Paying attention to safety concerns and physical barriers is essential for clients with brain injury. Need of a caregiver depends on the type of injury, level of injury, and independence level. Patients who have a brain injury or incomplete spinal cord injury may be in danger of wandering off, falling, or losing orientation. “Somebody who has paraplegia may be able to do everything on their own and be completely independent in an environment that’s set up for them,” says Jennifer Baribeau, OT, who works at Craig Hospital, Englewood, Colo. “If you have a higher-level patient, meaning a cervical-level patient with a spinal cord injury, they might not be able to do everything in their environment on their own,” she says. These individuals may need some modifications or help getting set up in their chair to fulfill the activities of daily living (ADLs).
Falls can be an issue after spinal cord injury or TBI. Aiming to create an environment that encourages independence and safety sometimes leads to mishaps for patients who do not know their limits, so occupational therapists consider all contingencies. Wandering can be another concern, but high and low tech solutions help keep tabs on patients. If the home has an alarm in place, the door chime can be set to ring when the door is opened, alerting family members, says Sara Meredith, OTR/L, an occupational therapist on the Brain Injury Team for Casa Colina. Many cell phones have GPS signaling capabilities, and using certain programs can trigger a text message if the cell phone goes outside of a certain range, Mackenzie adds. “If you have someone who is a little more independent, and you want to give them more freedom, they can use that device and it will alert their family if they go outside of a designated range,” she adds.
The elderly population, who may be more rooted in and attached to a home, may embark on modifications, mindful of sustaining the home’s integrity and resale value. “It can be a challenge, finding that happy medium that meets the patient’s physical needs but also meets their emotional needs,” says Amanda Carr, OTR, ATP, an occupational therapist who works with spinal cord injury patients at Craig Hospital.
 |
| Lifts enable aging and physically challenged individuals to more easily negotiate multiple-level homes. Shown above is the Bruno Custom Crafted Curved Stairlift, the Electra-Ride III (Model CRE-2100). Photo courtesy of Bruno |
LOOKING AHEAD
Basic needs will be addressed right away, but other wide-ranging options may be postponed. “We’ll make recommendations, and then once the patient gets home and is more settled, they’ll start to implement those things,” says Carr. A patient may not be able to access an upstairs bedroom right away, opting instead to sleep in the dining room for a few months while they accumulate funds for construction and assess the need. “You don’t necessarily want to put a lot of money into home modifications and then wind up not needing them in the long run,” says Carr, noting that patients can come back for reevaluations, or, if they live out of state, Craig therapists can connect them with local therapists for a home evaluation.
Considering the family when making changes and seeking harmony with caregivers are important. Does the group congregate in the living room or in the kitchen? How can all of the needs be accommodated, and what compromises are acceptable? Therapists spend a lot of time reminding family members to sit on their hands, and even though it may be easier and quicker for them to do a task for patients, they should often try not to intervene unless the task is unsafe, says Meredith. She says also that many home adaptations do not interfere with the functionality of the home and can actually increase the efficiency of activities.
Occupational therapists at Craig Hospital encourage patients to instruct caregivers and work with them for win-win results. “We work on setting up a routine before the patient goes home, so that the family and caregiver and patient can all work together to have the most effective and efficient method of having the home adapted and also getting their routines done,” says Baribeau. Compromise and consideration faced one patient who was discharged home and had to sleep in the living room, an arrangement that disrupted the family milieu. “They’re going to build a curtain, and she’s going to be in her living room until they can make other modifications,” Baribeau says. “It definitely does impact it, but at the same time, the person is at home with their family and they’re back in a more normal environment, which is a good thing. We always try to get our patients back with their husband or wife, or in a normal bed, or do whatever we can to make the situation as normal as possible, or as preinjury as possible.”
Future considerations also factor into the equation. “When we get patients who are high school- or college-level, it’s very expensive to modify your home and make it completely accessible, so we have to keep in mind that that age group is going to be evolving,” says Carr. “We need to make sure that our recommendations are going to be universal for the different settings they are going to—whether it is a college dorm room, or an apartment setting—and that the environment can change with them and their needs.”
The flux in changing needs can sometimes be stressful, but occupational therapists provide support. “One of the biggest issues is a family who has all of these extra burdens, role changes, tons of stuff going on at the moment, and they’re dealing with changes from all sides of life, and then they’re asked to modify or change their home too, which is usually somebody’s huge stability,” says Baribeau. “All of that, and the economic burdens from it, are huge factors.”
Carr notes that the lengths of hospital stay are getting shorter and shorter, and so there is less time for patients and their family members to prepare the house by the time they return home. “We have a lot of patients who are out of state, so it’s hard to be in two places at once, from most caregivers’ standpoint—to be with your loved ones for training and education, but then also to be at the house to make sure it’s safe and ready to go home to.”
SAFE AND SECURE
Occupational therapists may recommend security measures, such as installing door locks, alarm devices, ramps, and zero-step entrances—especially if a patient will be alone in the home at night. “This may be a keyless entry, having a lockbox, or having security cameras so the patient can see who’s ringing the doorbell,” says Carr. Her colleague Baribeau sometimes recommends a remote control for turning alarm systems on and off.
 |
 |
| Smooth flooring, widened doorways, and lowered work counters and appliances can accommodate the needs of wheelchair users. Photos courtesy of Accessible Systems, Inc. | |
AGING IN PLACE
Universal Design principles involve elements that make homes more user-friendly, whether aiding people who have balance, strength, cognitive, or vision deficits. As people age, they naturally lose some of their balance and hearing, so therapists must accommodate for those deficits, says Mackenzie.
Craig Hospital offers a reevaluation program for aging in place, where patients generally return in about 6 months, depending on the circumstances, to discuss needed changes. The facility’s brain injury program provides continuing outpatient therapy, and when therapists make home visits, they offer advice on better or safer options. In-home therapy reinforces skills taught in the hospital. “A lot of times with a brain injury, if [the patient has] cognitive deficits, putting it into the real-life situation is what makes the skills stick,” says Carr, noting that technological advancements may arise in the interim. “The patient, physically, might be in the same situation, but 6 months later they might come back and we can then offer them different things that might be more effective, less expensive.”
Sometimes challenges are needed within ADLs to advance patients’ progress. “Whether it’s a challenge to set up the sink so they can complete their grooming tasks—even if it is difficult for them—or making sure they can access the computer so they can complete their activities of daily living, our focus is to get the patient as independent as possible,” says Carr.
 |
|
 |
 |
| The Assistive Technology Center at Casa Colina, Pomona, Calif: A therapy garden, top, features ramps and sloped walkways; patient Theresa Montoya, left, works at an adapted computer station; kitchen space, right, is modified for easier access. Photos courtesy of Casa Colina | |
SUPREME CHALLENGE: FUNDING HOME MODIFICATIONS
Funding is often one of the biggest challenges when it comes to making modifications, because they can be costly, according to these experts. Health insurance rarely covers home modifications, unless it is through workers’ compensation. Scholarships and grants may be available through various organizations, and sometimes outside funding serves as a stepping stone in the right direction. Carr says making a major modification exerts a big burden in addition to all of the family’s other medical costs. Therapists recommend options based on the needs of the patient, from the least to the most expensive, and may modify the list or suggest less-costly alternatives, says Meredith. “From a funding aspect, it’s a huge thing to consider, because we’re making these recommendations for their home, but we’re also making recommendations for a lot of other equipment,” says Carr. “They have to be able to prioritize their funds and their situation as to what comes first. The home modification is more often done in stages than be 100% complete by the time the patient gets home. Because, from a financial standpoint, it’s very difficult to be able to pull that off.”
Baribeau urges people to consider untapped resources by asking, “Do you have any friends or family who are in construction, can do construction, want to volunteer, want to help?” She says. “That’s one of the huge things, getting the time, the manpower, and the supplies to make the modifications as needed.” Despite ongoing changes in the health care model, Mackenzie says the recession has not significantly impacted the availability of resources.
GETTING SET UP—PIECE BY PIECE
Patients often need a ramp of some kind, and perhaps two ramps, depending on the number of entrances and exits. For every 1 inch of rise going into a home, you must have 1 foot of ramp.
For people with spinal cord injuries, Baribeau often recommends a stairlift, or a roll-on lift. A suitable ramp may have a platform on the front so the person can open the door. “Ideally, the ramp would have guard rails on the side or a railing so if the person was driving a 300-pound wheelchair, they’re not going to go off the edge accidentally by making a wrong turn,” she says. “We have patients who drive their chairs with sip ‘n’ puff, and that’s their way of controlling an entire huge, heavy piece of equipment. We want to make sure they’re going to be safe and set up for the best environment possible.”
Options for the bathroom are numerous and fit most individuals’ needs. For example, strategically placed grab bars throughout are a must. For bathtub safety and ease-of-use, hydraulic, mechanical, and powered bath chair lifts are available. In addition, there are bathtub chairs in adult, bariatric, and child sizes, wheeled and reclining bath seats, and bathtub transfer boards to meet specific needs. Commode chairs are available in a variety of sizes and heights (including models with power and manually elevating features) to accommodate height, size, and weight. Those requiring assistance in the shower may appreciate a custom-made 5-foot by 5-foot roll-in shower with a flexible shower hose so they have enough space for themselves and a caregiver. If patients use a bench versus a chair or stool, they could keep their regular tub, and the bench would fit in the tub. Being able to get underneath the sink for greater access to the sink and the countertop is helpful (and this applies to the kitchen as well).
 |
| Wheelchair-friendly tile floors, accessible toilets, strategically placed grab bars, and handheld shower heads are among the myriad of modifications recommended for the bath. Photo above and below courtesy of Accessible Systems, Inc. |
Simple kitchen modifications can make a big difference, such as buying another microwave and placing it on a lower counter, or placing blocks under the kitchen table to create an accessible surface area for cooking prep. Sometimes it is preferable to have a side-by-side refrigerator, other times not. Protecting the piping below sinks helps prevent patients who cannot feel their lower body from burning themselves.
Offset hinges in doorways can carve out an extra inch of space, avoiding major construction. Lever door knobs and handles make it easier for patients to get in and out of their home. Also helpful are handrails and elevated beds, chairs, and sofas.
SAFE LIFTING AWARENESS
The safety of both patient and caretaker must also be considered when outfitting a living environment for special needs individuals. Safe patient lifting, transferring, and repositioning are a rising concern among caretakers, who are aware that injuries can occur to both them and their charges during the daily process that involves lifting someone from bed to toilet to bath/shower to chair. Fortunately, a variety of lifts and transfers are available to suit most environments, lifestyles, and circumstances, not to mention offering a safer, easier, and more comfortable transferring experience for patient and caregiver.
Basic patient lifts are ceiling- (or overhead-) mounted lifts and floor lifts. Professionally installed ceiling lift systems are mounted on permanent straight or curved tracks, and can offer access to multiple rooms, as well as lift options. Also, very little manual lifting by the caretaker is required when using a ceiling-mounted system. Often battery-operated, optional control features for this technology can enable a user to move independently, depending on physical abilities, throughout the home environment.
Floor lifts are available in a variety of models, including manual, hydraulic, or battery-powered, as well as stand-up, heavy-duty, and portable units. While each model provides a safer, more comfortable transfer experience for patients, each system offers unique features. Manual units require more involvement for caretakers, who still are very hands-on with the lifting process. Power systems reduce caregiver injuries, while providing the patient with a smoother transition. Heavy-duty lifts (usually power-controlled) often offer the capability of lifting individuals weighing as much as 1,000 pounds. Also, floor lifts are often more affordable than ceiling lifts, and many models offer portability and maneuverability in a variety of settings. (They can also provide a backup device for ceiling lifts.) Regardless of the system, be certain to carefully consider the needs and requirements of both patient and caretaker when making a purchase.
 |
ENVIRONMENTAL CONCERNS
TBI patients who are ambulatory might need more environmental prompts, such as putting up notices, or making things visually different so they can see contrast, says Carr. “They may not necessarily need the ramps, but make sure that the stairways are safe, maybe having grab bars on the side, and label big steps.”
Mackenzie also suggests the following: raised box gardens, rocker switches for lights, speaker phones, raised or lowered counters, voice-activated computer systems, track balls, Hoyer lifts or lifts in the ceiling, an automatic sink, tiled or wood floors in lieu of carpet, and high tech environmental control units to control the entire home from a computer.
Casa Colina’s assistive technology lab allows inpatients, outpatients, and those at its Transitional Living Center to be evaluated, try things out, and practice-especially those who need a lot of assistance. “High-level spinal cord injury patients might need an automatic door opener, or a computer system that allows them to access their home with an environmental control unit,” says Mackenzie. The lab features a variety of computers, environmental control units, computer access, adapted telephones, augmentative communication devices, track balls, and voice-activated recognition software that allows patients to talk and have a their whole house work for them. The products facilitate aging and a change in status.
Judy O’Rourke is associate editor of Rehab Management. She can be reached at .
Home Modification Contacts
Funding home modifications can be costly. These resources may help:
The Denver Home Builder’s Foundation often receives applications from Craig Hospital, and has completed many projects over the years. Applications can also be submitted directly by individuals. The staff at Craig has also contacted other chapters of the Home Builders Foundation nationwide and some have been in a position to assist. Each individual chapter operates differently.
In states that have an Elderly/Blind/Disabled Waiver Program (Home and Community Based Services), there is often a one-time allotment of $10,000 for home modifications. The amount varies from state to state and cannot be accessed until an individual is in the community. Individuals must meet the financial and disability requirement for Medicaid.
The AV Hunter Trust and Friends of Man is an option in Colorado. Applications are accepted only from referring professionals such as health care and social workers, clergy, counselors, etc. Nationally, The Volunteers of America operates a Handy Man program, which provides people to build ramping, but it does not cover the cost of supplies. The Travis Roy Foundation (www.travisroyfoundation.org) and SCORE (www.scorefund.org), for people with spinal cord injuries, help with DME, van modifications, adaptive athletic equipment, and more, and they will sometimes provide funds for modifications. People apply on an individual basis. Applications can be completed online.
Many times patients locate grants through the Center for Independent Living and the Department of Vocational Rehabilitation; however, each state differs in what can be offered and will have different qualifying criteria.
The NTAF (National Transplant Assistance Fund) has a Catastrophic Injury Program (www.catastrophicfund.org) designed to assist those who have sustained a catastrophic injury (spinal cord or traumatic brain) establish successful fundraising campaigns. The funds raised are for uninsured expenses related to catastrophic injury, including home modifications. The funds raised on behalf of individuals are tax deductible, and are administered by NTAF.
If an individual has had any active duty in the military during their lifetime, the Paralyzed Veterans Association (www.pva.org) can also assist with home modifications. Local chapters operate throughout the country.
Rural Housing Service (through the Department of Agriculture) and the AgrAbility Project (www.agrabilityproject.org) were created to assist people with disabilities who are employed in agriculture. They can assist with a variety of services, including modifications.
Through the US Department of Housing and Urban Development, various programs exist to help with loans (property improvement loans and rehabilitation loans) and grants for those who meet qualifying criteria.
The grants are overseen by individual states based on that state’s qualifying criteria. One should go through the municipal office in their area. Levels of funding and qualifying criteria differ from state to state.
[Resources courtesy of Stephanie Percival, director, Patient and Family Services, Craig Hospital]
WYNGS
www.wyngs.org
Home modifications up to $2,500; specifically for people with SCI.
The Jewish Free Loan Association (JFLA)
www.jfla.org
Home modifications up to $3,000, interest free loans. Must be a resident of Southern California.
[Resources provided by Claire Malawy, MA, OTR/L, Casa Colina]
Additional resources:
Brain Injury Association of America
www.biausa.org
(800) 444-6443
Centers for Disease Control and Prevention
www.cdc.gov
(800) 232-4636
Defense and Veterans Brain Injury Center
www.dvbic.org
(800) 870-9244
Health Resource and Services Administration
www.hrsa.gov
(301) 443-3376
National Association of State Head Injury Administration
www.nashia.org
(301) 656-3500
National Brain Injury Research Treatment and Training Foundation
www.nbirtt.org
(434) 220-4824
National Center for Medical Rehabilitation Research, NICHD, NIH
www.nich.nih.gov/about/ncmrr
(800) 370-2943
National Institute on Disability and Rehabilitation Research
www.ed.gov/about/office/list/osers/nidrr
(202) 245-7640
National Institute of Neurological Disorders and Stroke, NIH
www.ninds.nih.gov
(800) 352-9424
North American Brain Injury Society
www.nabis.org
(703) 960-6500
Social Security Administration
www.ssa.gov
(800) 772-1213
National Disability Right Network
www.ndrn.org
(202) 408-9514
San Diego Brain Injury Foundation
www.sdbif.org
(619) 294-6541
Betty Clooney Foundation
www.bcftbi.org//supportgroups.asp
(562) 938-9005
Coastline Community College, Acquired Brain Injury Program
www.coastline.edu
(714) 241-6214
Jodi House Brain Injury Support Group
www.jodihouse.org/links.htm
(805) 563-2882
Centre for Neuro Skills
www.neuroskill.com
(800) 922-4994
[Resources provided by Sara Meredith OTR/L, OT on the Brain Injury Team for Casa Colina]
More sources:
ILC: Independent Living Center of Southern California
www.ilcsc.org
Christopher and Dana Reeve Foundation – Paralysis Resource Center
www.paralysis.org
National Spinal Cord Injury Association (NSCIA)
www.spinalcord.org
[Resources provided by Claire Malawy, MA, OTR/L, Casa Colina]