By Tamara Kittelson-Aldred, MS, OTR/L, ATP/SMS, and Lee Ann Hoffman, OT, MSc.
While use of 24-hour posture care management as a systematic approach is quite new in North America, its roots were established in the 1980s with foundational work occurring even earlier. Initial discussions in the United Kingdom (UK) were documented in the 1970s, with Fulford and Brown marking a point in early intervention and awareness in their paper highlighting the need to prevent asymmetrical deformities in children with cerebral palsy and suggesting therapeutic positioning as a possible tool.1
Concepts and Approaches
In the United Kingdom, developments progressed within the field of posture care management for children with severe disabilities through work undertaken during the 1970s and 1980s by Noreen Hare, a physiotherapist. Hare developed the Physical Ability Scale (PAS), which can be traced back as the cornerstone for 24 hour posture care management. The PAS was expanded upon and became the foundation for the Chailey Levels of Ability that was developed for children and youth with cerebral palsy by Pountney et al.2
Following on from this, Pauline Pope developed the Posture and Postural Ability Scale (PPAS), which is an assessment tool used for individuals with severe physical disability, not limited by age or diagnosis. Her work focuses on physical management of posture as a foundation separate from treatment of chronic disabling conditions.3 The idea is that all people with motor impairments will experience the health benefits of having a better-aligned body through posture management regardless of whether or not they are able to make large functional gains in active therapies. Along with observations of postural asymmetries in young adults with cerebral palsy, Rodby-Bousquet et al have undertaken studies of the PPAS psychometric properties of reliability and validity for use in adults and children with cerebral palsy.4,5,6
Another prominent approach in posture care management is that of Liz and John Goldsmith, who focus on lying posture and distortion of the chest due to gravity.7 The foundation of all intervention in the Goldsmith approach is a focus on family and support workers providing intervention to protect body shape through appropriate positioning day and night. This approach holds the supine lying postural orientation at night as the gold standard for protecting and improving body shape.
Developments in the field of 24-hour posture care management have led to changes in policy and treatment interventions in many countries.8,9,10 These changes have brought offerings of more formal and accredited education in this area, for professionals and families/caregivers.11-14 Informed awareness of the benefits of protecting body shape through 24-hour posture care management is instrumental to the success of the approach. The three orientations available to human beings are lying, sitting, and standing. Sitting and standing are regularly and thoroughly discussed in the North American seating, mobility, and positioning practitioner world. Therefore, in this article we focus on lying posture as it is often overlooked as an orientation that may require intervention.
Gravity, Support, and Parallels Between Lying and Sitting
During the process of planning seating interventions, understanding the parallels between lying and sitting posture is crucial for long-term success. The similarity between lying and sitting posture is often noted during mat evaluations, but unfortunately is rarely the focus when seating systems are being prescribed. Overlooking this dynamic could become the missing link that will sabotage successful seating outcomes over time, resulting in modifications and earlier equipment replacement than would otherwise be necessary.
Gravity and asymmetrical positions are forces to be reckoned with during long hours spent unsupported while sleeping in bed or relaxing outside the wheelchair. If these postures are not analyzed and addressed constructively, the benefits of custom seating will be counteracted by unsupported, destructive positions that tend to occur. Time spent in lying, even for a full-time (12 to 16 hours per day) wheelchair user is significant, and far outweighs the time spent in therapies or in standing equipment.
For a person with impaired movement, postural asymmetry in lying can easily become obligatory over time. Preferred positions have many origins; muscle tone irregularities, reflex activity, lower body contractures from long-term sitting, sensory impairments, and other issues can all influence a person’s postural tendency in lying just as in sitting. In 1987 Noreen Hare described the “human sandwich”3—all people are constantly living and moving between the force of gravity and the support surface beneath us. A person’s body shape gradually accommodates to postures as they become habitual, and eventually the skeletal structure can change so that there are fewer postural choices. These eventually become obligatory—when unsupported, the person has no choice. Gravity coupled with asymmetry over a long enough period of time can lead to or worsen complications like pelvic obliquity and rotation, rib cage distortion, scoliosis, hip and other joint dislocations. Sometimes body shape can become so complex that posture becomes a mirror image of itself whether lying in supine or in prone, or in right- or left-side lying.
Success Essentials: Interdisciplinary Expertise, Shared Knowledge
Twenty-four-hour posture care management is an interdisciplinary approach, requiring input from professionals, the individual, and their support system. While seating and mobility practitioners are uniquely suited to assessing, observing, and understanding the interaction of sitting and lying postures, they may not be best placed for intervening on an ongoing basis. Families and direct caregivers who are consistently part of an individual’s life can support that person and implement 24-hour posture care management principles most effectively. Those who know an individual best are able to offer input as an integral part of the team when planning positioning interventions, since they will be implementing or assisting in the process on an ongoing basis.
This requires thorough education for all involved. Professionals, individuals, and their caregivers require knowledge as well as commitment to following the process of 24-hour posture care management. That process can be tricky when it involves changing personal habits such as sleeping and relaxing, and often requires incremental adaptations over time. Individuals and their caregivers must be able to make posture support adjustments and resolve problems that may arise at odd times of the day or night. Implementation of 24-hour posture care management is much more than just providing equipment. It requires assessment, goal setting, planning, implementation and follow-up—just like seating and mobility interventions.
Discussion
In North America 24-hour postural management is not well known, discussed, or commonly used as a standard of care compared to other parts of the world. Professionally, the use of evidence-based practice is emphasized strongly, yet there is a paucity of high-level research directly supporting the effectiveness of therapeutic positioning over 24 hours in a day, especially at night. In such situations, however, an evidence-informed approach is useful. As defined by Dodd and Savage, evidence-informed practice incorporates the best available research evidence with theory, client values and choices, and practitioner clinical judgement, into the decision-making process when planning interventions. This will always be “filtered through the lens of client, agency, and community culture.”15
With this in mind, there is a small but growing body of evidence discussing the effectiveness of posture care management. Two literature reviews about the subject have been recently published16,17 recommending more research. Publications from Pountney et al18,19 evidenced a reduction in hip subluxation and related surgeries in the cerebral palsy population; Porter reported the correlation between the directions of scoliosis, pelvic obliquity, and preferred posture in non-ambulant people with cerebral palsy20; and the “Mansfield Project” focused on hip health and management through night-time positioning and intervention in lying to protect body shape.13 Sato has documented prolonged periods of immobilization at night in children with cerebral palsy, suggesting that such children may benefit from “postural care assistance” at night.21
In addition, Pope provided 24-hour positioning interventions and applied these principles to both children and adults.3 Of note, Pope undertook posture management with adults diagnosed with multiple sclerosis, implementing positioning in lying as part of their treatment plan. Pope underpins the intervention of 24-hour posture care management by focusing on building a stable posture in lying, sitting, and standing.

Baseline measures of body symmetry can be monitored over time to assess effectiveness of the intervention.
Night postural care shares theoretical common ground with the use of custom seating systems, bracing and equipment such as standing frames that support a person’s body in alignment, symmetry and midline orientation to the extent possible. The difference being that night postural care is done when gravity can be more easily harnessed and muscle tone relaxes as part of normal sleep patterns. In this context understanding the dynamics of behavior change, sleep patterns, and willingness to weigh pros and cons of using night posture care management are essential tools for success.
Outcome measures are used to document the effectiveness of posture care management in lying as is done with any other intervention. Measures can include photos, the Posture and Postural Ability Scale, Goldsmith Indices of Body Symmetry (linear and goniometric measurements of chest symmetry and windswept postural tendency), ipsilateral and contralateral critical chest measurements, and others. The Postural Habits Assessment Tool is another useful interview instrument, from Lyndhurst Seating Clinic at Toronto Rehabilitation Institute.22 Sleep questionnaires and pain profiles have also been used to measure change. In addition, qualitative reports of daily function can be highly valuable in determining whether interventions are effective for an individual.
An evidence-informed, eclectic approach to 24-hour postural management can be implemented in practical ways by families and caregivers. Successful use requires understanding the forces of gravity acting on the body while lying, the relationship between lying posture and function in sitting and standing, dynamics of behavioral change, setting of appropriate goals and timelines, and other subtleties. Analyzing risks versus benefits and problem-solving to find solutions are essential when undertaking night posture care management for individuals who have complex impairments and needs. With the appropriate knowledge, and often inexpensive everyday materials, it is possible to plan night-time positioning interventions that will work toward supporting daytime success. Sleeping posture in the night can then work in harmony with daytime seating systems rather than counteracting them.

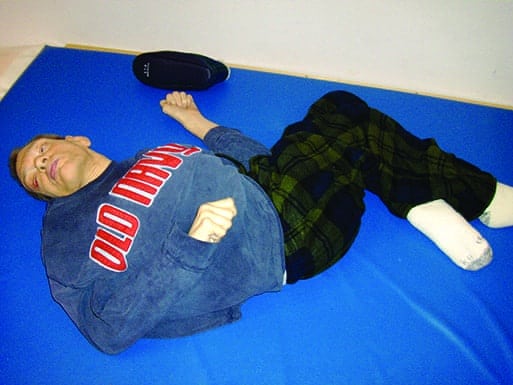
Corrected supine postures without and with support. Sleep system provided better correction than a body jacket that was interfering with sleep.
Practical Aspects
Supporting a person in lying is often easier than in sitting, because gravity is more readily harnessed in a constructive way. Supine lying as an ideal allows for symmetrical support to protect or correct posture most easily because rotation around the body’s longitudinal axis can be controlled. Providing lateral support at the hips and trunk often feels comforting for people with poor ability to lie in balance or those with postural insecurity. Adding support beneath the knees often helps those with hip and knee flexion contractures by allowing them to rest with their legs oriented in better midline symmetry rather than falling to one side or the other, as is commonly seen. This reduces strain on hip joints and distorting effects on the rib cage, and improves comfort. Of course, the degree of correction possible in people with established distortions must be carefully determined and will often require gentle, gradual change over time. Even people with complex body shapes who may not have very correctable posture can experience increased comfort in lying and slowed progression of problems they already have. This can be done by providing support for their posture “where they are,” promoting relaxation and a feeling of security.
Side sleeping is often used because of concerns about breathing, aspiration, and digestion. Side and prone sleeping can be more destructive postures secondary to the difficulty of managing rotation around the longitudinal axis of the body, and (in prone) the extra weight of the spinal column on top with the malleable rib cage and internal organs beneath. However, many people have been able to transition to supine sleeping when the process is planned carefully to account for safety and implemented gradually. When that is impossible, careful support of the person in as much symmetry as possible is the goal, again trying to limit rotation of the person’s body around its longitudinal axis.
Frequent turning side to side is also common in order to counteract pressure injury risks. However, this often introduces rotation and sleep disruption. Interestingly, pressure mapping often reveals improved pressure distribution with the addition of lying supports. In some cases individuals who were thought to be at high risk for developing pressure injuries at the sacrum have safely transitioned to a supported supine sleeping posture with no skin breakdown resulting.
In North America the Montana Postural Care Project has been funded by the Montana Council on Developmental Disabilities since 2016. Results from the first year cohort were positive within 5 to 6 months of beginning interventions, based on measures of body symmetry, sleep quality and pain.23 Of those who implemented night posture care management even part-time, nearly 80% experienced improved sleep quality and more than 80% showed improvement in some aspect of body symmetry. More than 50% of those for whom pain was an issue exhibited lower pain scale scores. In no case was improvement seen in any of these areas for those who did not implement night therapeutic positioning.
Posture care management has promising potential, but North American awareness is still in early stages. If body shape distortions such as scoliosis, pelvic obliquity/rotation and joint dislocations can be limited or avoided noninvasively with therapeutically supported postures used around the clock, it is good news. If body shape can be improved toward symmetry while supporting better sleep and reducing pain, the news is even better! RM
Tamara Kittelson-Aldred is an occupational therapist, Assistive Technology Professional/Seating and Mobility Specialist. She earned certificates in advanced postural care through the Open College Network West Midlands in England. She directs the Montana Postural Care Project, promoting postural care and responsible wheelchair provision. Kittelson-Aldred has written and presented on these topics in the United States, Jordan, and Peru, and has served individuals with complex neurodisabilities in Montana since 1983. She credits her daughter Eleanore, born with cerebral palsy and profound deafness, as her best teacher.
Lee Ann Hoffman, B.Occ.Ther (RSA), MSc. Rehabilitation, has a specialized interest in the 24-hour posture management approach and its effects on quality of life. She has worked internationally in several different healthcare settings with individuals who have complex rehabilitations needs. She obtained a post-graduate certificate in posture management for complex disabilities, and a Master of Science in Rehabilitation: posture management. Hoffman is a member of Invacare USA’s Professional Affairs and Clinical Education team. For more information, contact [email protected].
References
1. Fulford GE, Brown JK. Position as a cause of deformity in cerebral palsy. Dev Med Child Neurol. 1976;18(3):305-14.
2. Pountney TE, Green E, Mulcahy C, Nelham R. Chailey levels of ability. Physiotherapy. 1999;85(12):693.
3. Pope P. Severe and Complex Neurological Disability: Management of the Physical Condition. 2007;Butterworth-Heinemann Publishers.
4. Rodby-Bousquet E, Czuba T, Hägglund G, Westbom L. Postural asymmetries in young adults with cerebral palsy. Dev Med Child Neurol. 2013;55(11):1009-1015.
5. Rodby-Bousquet E, Ágústsson A, Jónsdóttir G, Czuba T, Johansson AC, Hägglund G. Interrater reliability and construct validity of the Posture and Postural Ability Scale in adults with cerebral palsy in supine, prone, sitting and standing positions. Clin Rehabil. 2014;28(1):82-90.
6. Rodby-Bousquet E, Persson-Bunke M, Czuba T. Psychometric evaluation of the Posture and Postural Ability Scale for children with cerebral palsy. Clin Rehab. 2016;30(7):697-704.
7. Hill S, Goldsmith J. Biomechanics and prevention of body shape distortion. Tizard Learning Disability Review. 2010;15(2):15-29.
8. Crawford S, Stinson M. Management of 24 hour body positioning. In: Söderback I, Ed. International Handbook of Occupational Therapy Interventions. 2015: Springer International Publishing Switzerland; 189-203.
9. Gericke T. Postural management for children with cerebral palsy: Consensus statement. Dev Med Child Neurol. 2006;48(04):244.
10. Wynn N, Wickham J. Night-time positioning for children with postural needs: What is the evidence to inform best practice? Br J Occup Ther. 2009;72(12):543-550.
11. Bacon H. Does a postural management training programme improve understanding of the importance of postural management for children with complex movement disorders? APCP. 2013; 4(1):27-36.
12. Castle D, Stubbs B, Clayton S, Soundy A. A 24-hour postural care service: Views, understanding and training needs of referring multidisciplinary staff. Int J Ther Rehab. 2014;21(3):132-139.
13. Goldsmith S. The Mansfield Project: postural care at night within a community setting: a feedback study. Physiotherapy. 2000;86(10):528-534.
14. Humphreys G, Pountney T. The development and implementation of an integrated care pathway for 24-hour postural management: a study of the views of staff and carers. Physiotherapy. 2006;92(4):233-239.
15. Dodd SJ, Savage A. Evidence-informed social work practice. In: Encyclopedia of Social Work. doi:10.1093/acrefore/9780199975839.013.915
16. Blake SF, Logan S, Humphreys G, et al. Sleep positioning systems for children with cerebral palsy. The Cochrane Library. 2015.
17. Robertson J, Baines S, Emerson E, Hatton C. Postural care for people with intellectual disabilities and severely impaired motor function: A scoping review. J Appl Res Intellect Disabil. 2016.
18. Pountney T, Mandy A, Green E, Gard P. Management of hip dislocation with postural management. Child Care Health Dev. 2002;28(2):179-185.
19. Pountney TE, Mandy A, Green E, Gard PR. Hip subluxation and dislocation in cerebral palsy–a prospective study on the effectiveness of postural management programmes. Physiother Res Int. 2009;14(2):116-127.
20. Porter D, Michael S, Kirkwood C. Is there a relationship between preferred posture and positioning in early life and the direction of subsequent asymmetrical postural deformity in non-ambulant people with cerebral palsy? Child Care Health Dev. 2008;34:635-41.
21. Sato H, Iwasaki T, Yokoyama M, Inoue T. Monitoring of body position and motion in children with severe cerebral palsy for 24 hours. Disabil Rehab. 2014;36(14):1156–1160.
22. Gauthier A. “Re: PHAT”. Received by Tamara Kittelson-Aldred. 29 September 2015. Email interview.
23. Kittelson-Aldred T. The Montana Postural Care Project: A 24 Hour Postural Care Model. 35th International Seating Symposium Proceedings. 2017:177-179.









this is great information. It is nice to have other’s doing similar stuff