Dynamic seating options for pediatric wheeled mobility help build greater levels of independent function for young users.
Carrie was a 5-year-old girl who had a diagnosis of schizencephaly and a severe visual impairment. Her case provided an entryway for me into the world of dynamic seating. The following article describes Carrie’s condition, recalls the process used to understand her seating needs, and introduces the options and benefits associated with dynamic seating for the pediatric mobility user.
CARRIE’S CASE
Several distinct characteristics could be observed about Carrie as a result of her condition. For example, upon hearing her mother’s voice, Carrie would turn to the direction of the voice and smile. Carrie liked to bang on a tabletop with her left hand—tending to keep her right hand in a fist. Another characteristic of Carrie’s behavior was that in school she would make noises when other children in class spoke to her or sang songs. She also demonstrated great enthusiasm toward snack time, and would attempt to take food that was placed in her left hand to her mouth.
Through collaboration with the vision specialist who worked at Carrie’s school, we determined that Carrie could see items move through her visual field only when there was bright lighting behind the item. Carrie would often lie on the floor by the large windows in the classroom during treatment. She could move her head to orient to items briefly, but did not reach for toys unless initiated by an adult.
When Carrie sat in her seating system, she leaned forward so far that her forehead almost touched her thighs. We used a cutout table during snack time, and tried placing food on her left side. Carrie would bang on the table, often sending the breakfast snacks or crackers flying. Because of her visual impairment, items typically used at school such as crayons, finger paints, and puzzles had no significance for her. Carrie would hold an object and bang it on the table two or three times before throwing it to the floor.
Signs of success began to emerge while Carrie was seated in my lap in front of a window, and we would rock gently from front to back. In this position, I noticed I could place her hand over a snack, then she would pick up the snack and successfully maneuver it to her mouth. At this point, she also began holding her sippy cup with both hands and lifting that to her mouth. Encouraged by these gains, we would transition back to her seating system and try the same task. This move met without success, and resulted in Carrie banging on the table and leaning forward. To solve this problem, we tried tilting her seating system back, but Carrie would pull her head forward off the headrest and sit motionless. She would not bang the tabletop or even attempt to take food placed in her hand and try to eat it.
Carrie had outgrown her seating system and her case manager asked if we would help the family obtain a new one for her. It was a fortunate coincidence that at about that same time a provider and representative asked to in-service our staff about a product with “dynamic seating.” Although the in-service focused on the concept that children with tone benefited from a seat and back that had springs and allowed for extension through the hips, we immediately thought of Carrie. After obtaining a demo, it quickly became evident that Carrie enjoyed the movement this new seating system allowed.
Carrie had predominately low tone yet would push herself back and forth in the dynamic seating system. She sat with her back in contact with the back of the seating system, and began to hold her head in an upright and neutral position. Carrie also opened her right hand and would place it on the table. She began to search for food with her left hand on the tray, and was able to place six to 10 small snack items to her mouth independently. The speech therapist who worked with Carrie reported that her random sounds began to have meaning. Carrie would actively say “mo” to request additional snacks or drinks. Observing these changes, the staff pursued this seating system and successfully provided it to Carrie and her family.
DYNAMIC SEATING BENEFITS
Independent and supported movement through dynamic standing and gait trainers is being linked with improved overall development in infants and toddlers.1 Dynamic standing programs improve bone mineral density. Increased bone mineral density means a child can have up to four times fewer fractures without trauma. Standing programs also increase range of motion at the hip, knees, and ankles, which makes transfers and self-help skills easier for the child and caregivers to perform.
Walking with the use of a gait trainer also is being linked to improved gross motor, fine motor, cognitive, and social skills in children with moderate to severe disabilities.1 Gait training can begin as early as 9 to 15 months. Supported movement, even in a gait trainer, allows a child to experience grounded exploration of the environment. The ability to move toward parents, siblings, toys, pets, and remote controls provides concrete knowledge of what is fun and what has consequences.
In addition to early standing and walking experiences, dynamic seating can allow moderately to severely involved children with both low and high tone to provide self-regulation, initiate pressure relief, and improve orientation of the body in space while in a wheelchair.2
OPTIONS FOR PERFORMANCE AND FLEXIBILITY
The term “seating system” refers to the seat and back components on a wheelchair that facilitate postural support, function, and skin integrity.3 The dynamic seating system that Carrie used had springs between the seat and back that allowed her to extend through her hips, open the seat to back angle, and return to an upright posture. There are seating systems that not only allow the seat angle to open but also the rear of the seat to lift in order to support the pelvis as the hips extend. This allows the seating system to remain in contact with the child as she moves and keeps the pelvis in a neutral orientation once the child returns to a seated position.
Wheeled mobility can be used for children in dependent systems and through self-propulsion. Dependent systems have smaller wheels and are pushed by another individual. Self–propulsion occurs when the child pushes on the wheels of the chair to move herself through space. Both systems can include static or dynamic seating systems on a 4-wheeled, 3-wheeled, or hi/low base. Many of these seating systems can be removed from the base for easier transport in a vehicle. The 4-wheeled and 3-wheeled bases often fold. The hi/low bases are used in homes and schools so a child can be close to the floor with same-aged peers or at the height of tables at school or in the home.
Static and dynamic seating systems also can be found on a stroller base. Strollers are one piece and fold with the seating components still integrated into the frame. Strollers can be more accepted by a family because they look similar to conventional strollers used for normally developing peers.
Additional seating components often found on dependent mobility manual wheelchairs include recline and tilt-in-space. Recline is an option where the angle between the seat and back can be opened or closed, while the angle between seat and ground remains the same.
Tilt-in-space is an option in which the seat angle orientation to the ground can be changed while the seat to back angle remains constant. Dynamic seating options also can be integrated into a system with tilt-in-space.
WHEELCHAIR CHOICES
Manual wheelchairs designed for self-propulsion are classified into folding frames and rigid frames. Folding frame manual wheelchairs fold in half at a cross brace in the middle of the frame. Folding frame chairs are not as energy efficient and take more effort to propel. However, they are easier to transport for families who travel and must store the wheelchair in a vehicle while driving. Rigid framed wheelchairs are welded and do not fold. They often come with folding back canes to decrease the overall height during transportation.
Although walking remains the preferred method of mobility, children with moderate to severe physical impairments often have to develop mobility skills in a seated position. Self-propulsion in a wheelchair allows for free exploration of the environment. Dynamic seating options are also available on certain self-propulsion frames. For some children, self-propulsion in a manual wheelchair is faster than independent or supported ambulation.
Even the lightest pediatric manual wheelchairs are a significant proportion of a young child’s weight. A wheelchair weight of 25 or even 34 pounds may be insignificant in comparison to the weight of an adult, but even a 15-pound ultralight manual wheelchair may be 30% of a 4-year-old child’s weight. The RESNA Position on the Application of Power Wheelchairs for Pediatric Users4 also lists difficulty with ergonomically correct axel placement, repetitive use injury, difficulty with head and neck control in a tilted position, and fatigue as major inhibitors to propelled mobility for children with disabilities.
Powered mobility for children with moderate to severe physical impairments has been advocated at earlier ages. The RESNA position states: “When looking at children driving a powered wheelchair, we need to determine what is meant by ‘driving’ and our expectations for these children. Normally developing children start exploring their environment at 3 to 4 months of age via reaching and rolling. Creeping at 7 to 9 months of age allows discovery of further distances, with resultant changes in perceptual, cognitive, and socioemotional behavior. At 12 to 13 months, children typically begin to walk. Therefore, utilization of powered mobility at similar ages is also recommended for the appropriate children, to enable them to explore the environment and in turn continue to develop motor and cognitive skills.”4
Pediatric power wheelchairs can cost $6,000 and more. Seating systems can be found as small as 6 x 6 inches. However, there is additional expense in “growing” these small seating systems as a child becomes taller and increases in weight. Many power wheelchairs are also adult-sized bases with smaller seating systems. The larger bases do not imitate the small footprint of a 1- to 3-year-old child. Finally, power wheelchair bases are not part of “normal development.” Interactions of children in powered mobility with their normally developing, same-aged peers are inhibited by the medical device surrounding the child who is affected by a disability.
A new power mobility option has been introduced, known as the modified ride-on toy car. These devices can be found at local toy stores. Toy cars often cost less than $200 and can require less than $200 to modify with supported seating and drive controls. These toys are relatively lightweight and small, and often are manufactured in designs that can be easily transported by parents. The child-friendly, colorful toy designs and the various toy functions, which may include headlights, voices, and car noises, likely make these toys more acceptable to adults and children than some other mobility devices. This may be an important consideration for therapists who want to begin early power wheelchair training with families who are hesitant to discuss power options.
MOVE TO LEARN—LEARN TO MOVE
Children with disabilities do not follow standard developmental milestones for physical, cognitive, and communication skills. Whether therapeutically observed or in clinically controlled research studies, the benefits of independent movement continue to be explored. Therapists are researching the connection between self-initiated movement and progression of overall developmental skills in cognition, social, speech, fine motor, and gross motor areas. It seems that we need to move to learn every bit as much as we need to learn to move. RM
Michelle Fox-Hustwaite, MA, OTR/L, ATP, received a master’s degree in occupational therapy from the University of Southern California. She has specialized in sensory integration and assistive technology for individuals of all ages, and also educates therapists and providers about adaptive equipment. For more information, contact [email protected].
[sidebar float=”left” width=”500″]
Sidebar: Write LMNs Like You Mean It
Every state and every insurance has different guidelines for what they want in a Letter of Medical Necessity (LMN). It is important to know them before you begin work. Contact your local guru; your local equipment clinic person, it might be the APTA or AOTA reimbursement representative or your state representative from your association. Almost every manufacturer also has someone who can help you. Don’t be a lone wolf, you need to know what you are up against. My biggest gift to you is a quote from the film, Forrest Gump, in which the title character states: “Stupid is as stupid does.”
Write a clear concise LMN with only the relevant necessary information. You are demonstrating medical necessity. Stick to that, and make the first step of choosing a medical necessity. It’s best if you choose an International Classification of Function (ICF) category and use its matching code. This makes the therapist appear to speak the funder’s language. Funders like that. For example, go to http://apps.who.int/classifications/icfbrowser and select “Child and Youth – English” or whichever one works best for the client. Then click on the little “plus” icons and select a medical necessity such as “bowel function.”
To illustrate this example, consider that I am writing an LMN for Ben to get a stander. I look under the categories and decide for this child his medical reason for standing is bowel movements. When 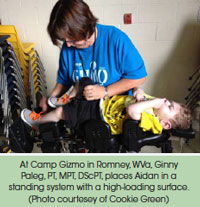
Once you have the score, perform another Internet search for “GMFM and percentiles” and find where their score fits best. This number (1-5) is the child’s Gross Motor Function Classification System (GMFCS) Level. Including this in the LMN conveys prognosis—the exact statistical chance that the child will ever improve enough to not need the device, and also the likelihood of contracture, dislocated hips, and scoliosis. Just about every child at Levels 4 and 5 needs a stander for their entire life. For a child at Level 3, they usually need a gait trainer until age 3 years and then again around age 16 years. Ben is a Level 5, so I shouldn’t have any trouble getting him a stander. These levels are our common language to show medical necessity.
The last part is: do not simply accept rejection. Do not accept that you can only get a stander or a gait trainer, but not both. If both are medically necessary, fight for both. You, the treating therapist. You fight. The buck stops with you. “We don’t pay for both” is not OK. Get the studies that show different medical benefits of each device. Pick one kid and fight. Get help. E-mail me and I will help you assemble an army.
So here’s my Forrest Gump plan. Take the time to write a really good letter about that specific kid (templates will trip you up!). Use all your best big medical words and tools (such as ICF and GMFCS). Leave out anything emotional, or anything that is not about that kid. Write what has been tried and why it did not work, as well as what you tried and exactly why it worked. If Ben does not stand in this stander that goes fully upright, his bowels do not move. When his bowels do not move, his blood pressure shoots up and he is in terrible pain and usually has to be hospitalized for 1 week or more. This is exactly what happened on all four occasions when he stopped using the stander—which he has now outgrown. In fact, it happened during the 4 months it took for me to find out that the funder rejected my request. It cost them $40,000 for his hospital stay instead of paying $6,000 for the new stander. Forrest Gump said, “Stupid is as stupid does.” Stand up for your clients and get them what they need. It is their basic human right to have the appropriate medical necessary equipment.
Ginny Paleg, PT, MPT, DScPT, is a pediatric physical therapist from Silver Spring, Md. For the past 11 years, she has worked for her local school system in its early intervention program. She earned a master’s degree in physical therapy at Emory University and her DScPT at the University of Maryland, Baltimore. She is a member of the editorial board of Rehab Management, and a member of the APTA, for which she served as a state representative and reimbursement specialist. In 2013, she was appointed by her governor to the Maryland Insurance Commission Habilitation work group. Recently, she has published four articles in peer-reviewed journals; two on standing (Journal of Pediatric Rehabilitation Medicine, 2011, and Pediatric Physical Therapy, 2013) and two on power mobility (BJO, 2013, and DMCN, 2014). She will present a symposium at the World PT Conference in Singapore (May 2015) about early mobility. She can be reached at [email protected]
[/sidebar]
References:
1. Paleg G. An Evidence Based Approach to Standing and Walking for Children with Moderate to Severe Motor Dysfunction. 2014 ISS presentation
2. Eason S. Dynamic Seating Why, Who & How. 2012 ISS presentation
3. Arledge S, Armstrong W, Babinec M. RESNA Wheelchair Service Provision Guide. 2011.
4. Rosen L, Arva J, Furumasu J. RESNA Position on the Application of Power Wheelchairs for Pediatric Users. Assist Technol. 2009;21:218–226.
5. Huang H, Galloway C. Modified ride-on toy cars for early power mobility: a technical report. Pediatr Phys Ther. 2012:24:149–154.





