E-stim is a modality commonly used for pain management in the outpatient setting, and it works by delivering an appropriately selected frequency and duration of electric current to help minimize the amount of pain a patient feels.
by Christen Biskelonis, PT, DPT, and Cara Yezzi, PT, DPT
Part 1: Outpatient Care
By Christen Biskelonis, PT, DPT
How many of us, patients and therapists alike, wake up each morning with general stiffness, aches, or pains? Probably more than you think; there are roughly 50 million Americans currently living with pain in the United States.1 There are numerous resources available to those individuals that assist in managing this pain, one avenue being outpatient physical therapy. In outpatient therapy clinicians treat a variety of patients with diagnoses ranging from orthopedic injuries to traumatic brain injury, multiple sclerosis, Parkinson’s disease, etc. Many of these patients arrive with some form of pain; it is our job as clinical healthcare professionals to assist these patients in finding the appropriate form of pain management.
Managing Pain in the Outpatient Setting
Many patients arrive to outpatient physical therapy secondary to an injury they sustained or postoperatively; both of these scenarios involve acute pain, which is a primary focus to address prior to then focusing on a patient’s strength, range of motion, and functional limitations. For acute pain in an outpatient setting, physical therapists must use their clinical reasoning skills to decide best practice in management of these symptomatic complaints. Passive services involving various types of modalities (heat, cryotherapy, electrical stimulation, ultrasound) can be used as an adjunct, but should not be the only avenue a therapist utilizes in pain management.
Working with Modalities
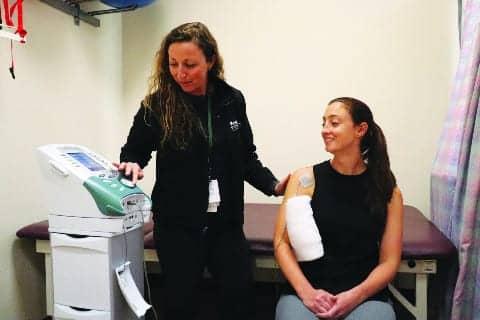
Each modality has its own benefits for short-term use. For example, electrical stimulation (e-stim) can be used for neuromuscular re-education or for pain management. Given the topic of pain management, transcutaneous electrical nerve stimulation (TENS) can be used as an adjunct in assisting a patient in reducing symptomatic complaints. Such types of diagnoses that could benefit from use of TENS are patients with orthopedic dysfunctions, specifically postoperative back, knee, or shoulder surgery. As a reminder, we as skilled clinicians should always review a patient’s medical history to ensure there are no contraindications or precautions to using electrical stimulation prior to use. If there are any uncertainties, communicating with the referring physician or surgeon is always recommended to ensure safe patient care is provided.
Manual Interventions
Beyond the use of modalities, with all physical therapists requiring multiple hours of continuing education to maintain licensure, our knowledge and training can provide even more options in the treatment of acute pain such as manual interventions involving soft tissue mobilization (hands-on or instrument assisted soft tissue mobilization-IASTM), various grades of joint mobilizations (specifically grade I/II), passive range of motion, and passive/manual stretching to improve flexibility and muscle extensibility. It requires careful consideration and attention from a skilled physical therapist in appropriately addressing acute pain so as to ensure a patient does not develop allodynia or hyperalgesia, which then can lead to chronic, debilitating pain.
Allodynia, which is a painful response to a normally non-painful stimuli, can be a barrier to rehab requiring treatment in and of itself involving various desensitization techniques such as gentle tapping, rubbing, or strumming the affected area on a patient with materials they can tolerate (for example: silk or cotton and as a patient’s tolerance improves, progressing to coarser materials such as jean or sandpaper). Hyperalgesia is an abnormally increased sensitivity to pain. It can develop from a chemical change in our neuroanatomy but also can develop from opioid use.
A major push in our profession as physical therapists is to encourage patients to explore alternative forms of treatment for pain rather than focus only on opioid medications, which have triggered an ongoing epidemic of misuse. If a patient participates in prolonged opioid use hyperalgesia can develop, which can create another barrier to their rehabilitation progress. This hyperalgesia can also lead to the development of chronic pain dysfunctions.
Chronic Pain: Outpatient Approach
Chronic pain is addressed differently in an outpatient setting from acute pain. As our facility also has a pain management physician on staff, our goal with chronic pain patients is to focus on function and mobility rather than their pain. Treatments that are commonly recommended for this patient population involve aerobic activity, flexibility and stretching, and low-load, low-impact strengthening. These types of activities help to reduce stress on joints and other passive structures, increase circulation and blood flow, and allow for increased ease in safely completing activities of daily living.
Pain is something that affects many people, but learning how to live with pain helps provide patients with a priceless tool that gives them a sense of control over their lives again as well as a sense of independence. Physical therapists are wonderful adjuncts who can help patients to learn how to manage their symptoms and live a successful, healthy, full life.
Part 2: Inpatient Care
By Cara Yezzi, PT, DPT
In the acute rehabilitation setting, many patients who therapists treat are suffering from acute and/or chronic pain. The interdisciplinary approach in this setting focuses on addressing our patients’ pain-management goals in addition to their personalized therapy goals. Our medical team assesses the pharmacological interventions for pain with recommendations from the skilled therapists on the timing of these interventions in order to maximize the performance of patients. Due to the complexity and acute level of the patients seen in this setting, more frequent assessments of pain and a variety of pain-management strategies are offered to reduce the potential for neurohumoral changes, neuronal remodeling, or emotional/psychological distress that could develop into opioid dependency or the development of chronic pain.
Applying Scales and Assessing Pain
The pain assessment scales utilized in this acute rehabilitation setting are the Visual Analog Scale (VAS), FACES scale, and the Face Leg Activity Cry Consolability (FLACC scale). The FACES scale is a set of six faces depicting a variety of severities of pain, which is a useful tool in treating patients who have difficulty with communication due to cognitive limitations or speech impairments such as aphasia. The FLACC scale is helpful in assessing pain among those patients with altered arousal states including those with disorders of consciousness, altered mental status, or even a patient who is asleep as this scale correlates observable signs of distress with a three-point rating scale.
Pain is assessed with every interaction the clinical staff has with each patient and re-assessed daily by therapists and every 12 hours by nursing. The skilled clinician also makes referrals for psychology and use of recreational therapy to further develop positive coping strategies for patients’ pain. It requires clinical reasoning to select individualized and effective pain management techniques that a clinician uses, being mindful of multiple contraindications/precautions such as cancer, blood clots, pacemakers, pregnancy, and skin integrity for many of the physical agent modalities including moist heat, electrical stimulation, and cryotherapy.
With the exception of ice, use of the modalities listed above require a written order from the rehab physician. Frequent skin checks are completed and documented when using modalities to ensure a patient’s tolerance to the modality. Cryotherapy and moist heat should be applied for between 15 and 20 minutes to achieve a true analgesic effect. Other supplemental non-pharmacological pain management strategies include: positioning, exercises, stretching, rest/relaxation, distractions, education, and canine therapy.

The FACES scale can ID the location and severity of pain with patients with aphasia and other communicative/cognitive limitations.
Gate Control Theory
There are different theories behind the analgesic effects of modalities, with one in particular that is referred to as the Gate Control Theory. Have you ever hit your foot on the side of a dresser? If so, you probably noticed how it begins to feel better once you sit down and rub the surrounding area of your foot Our pain receptors are small nerve fibers and our “normal” nerve fibers are larger. Both nerve fibers communicate to the projection fibers in the spinal cord, which will send a signal to the brain that pain is either present or absent. The more large nerve fibers on the projection fibers “close” the gate, or simply put, signal the brain that pain is not present. When the projection fibers receive more signals from the nociceptors (or pain receptors), this “opens” the gate, therefore signaling to the brain that pain is present. One way to help “close” the gates is to provide “normal” somatosensory input by use of tactile feedback or modalities.²
Pain Considerations at Discharge
The clinician’s primary goal in the acute rehabilitation setting is to maximize the participation and function of each patient as a way to promote a safe and independent transition home. Education about the surgical procedure or traumatic event as an adjunct to treatment plays another significant role in a patient’s pain management plan in this setting. The patient is admitted to the acute rehabilitation facility for as few as 48 hours or as long as 4 months, with a varied amount of education received prior to admission to the acute rehabilitation setting. The patient’s response to pain can improve with education about their current procedure and/or diagnosis as their expectations and understanding increases.¹ It is not uncommon that our patients discharge from the facility with persistent reports of pain, which is important for our patients to know so they may continue to seek skilled therapy and medical care upon discharge.
The opioid epidemic and pain management techniques are very important issues that the healthcare industry is currently addressing. Physical therapy plays an integral role in providing interventions, education, and resources for patients. RM
Christen Biskelonis, PT, DPT, is a Senior Physical Therapist at Kessler Institute for Rehabilitation based in Chester, NJ. She works in their outpatient department and treats a variety of patients from pediatrics to geriatrics and orthopedic patients to patients post-TBI or post-stroke. She has seven years of clinical experience, all at this location, and she also has a special certification in the LSVT BIG program for patients with Parkinson’s Disease.
Cara Yezzi, PT, DPT, is a Senior Physical Therapist at the Kessler Institute for Rehabilitation in Chester, NJ. Her main focus is in the inpatient department throughout her seven years with the company, but also consistently covers in the outpatient setting within the Kessler Division. She treats a variety of patients from geriatrics, orthopedics, traumatic brain injury, stroke, multiple sclerosis, Parkinson’s disease, and other neurological disorders. Yezzi is a Board-Certified Clinical Specialist in Neurologic Physical Therapy, a faculty member of the Kessler Neurologic Residency program, and has her LSVT certification in the treatment of Parkinson’s Disease. For more information, contact [email protected].
References
1. Dahlhamer J, Lucas J, Zelaya C, et al. Prevalence of Chronic Pain and High-Impact Chronic Pain Among Adults — United States, 2016. Morb Mortal Wkly Rep. 2018;67:1001–1006. DOI: http://dx.doi.org/10.15585/mmwr.mm6736a2
2. Moayedi M, Davis KD. (2013, January 1). Theories of pain: From specificity to gate control. Available at: https://www.physiology.org/doi/full/10.1152/jn.00457.2012. Accessed July 2, 2019.
3. Louw A, Diener I, Butler DS, Puentedura EJ. The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Arch Phys Med Rehabil. 2011;92(12):2041–2056.