
New technologies developed for pressure mapping systems have opened the doors to new applications and expanded pressure mapping benefits beyond the traditional seating assessment, offering therapists the opportunity to identify previously unnoticed issues.
by Kirsten N. Davin, OTDR/L, ATP, SMS
The application of pressure mapping has long been a beneficial technology in the seating and positioning realm, traditionally assessing the compression force between the seating surface and a client’s contact area. Recent research has emphasized not only the importance of incorporating this pressure analysis into the overall seating assessment, but also the value it holds in troubleshooting and identifying potential seating or pressure issues. Lesser known, yet of notable, perhaps even greater importance, is the relationship pressure mapping has with other seating accessories, including but not limited to anterior trunk supports, lower-extremity supports, pelvic rotation, obliquities, and other asymmetries found in the wheelchair seating arena.
Whereas the implementation of pressure mapping in regard to pressure assessment with wheelchair cushions is well-known, this article will shift the focus to the direct correlation between pressure mapping assessment and the variety of other wheelchair components and accessories that contribute to ideal positioning, pelvic control, and successful wheelchair seating and positioning.
[sidebar float=”center” width=”250″]
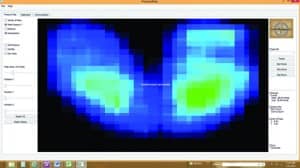
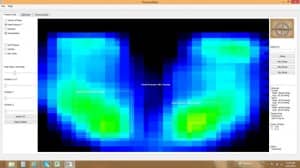
(top to bottom) Photo 1: Baseline pressure mapping images are helpful for clinicians to obtain a baseline presentation of the client and identify any asymmetries which may not be readily visible to the naked eye. Photo 2: Manual repositioning of a correctible posterior pelvic tilt can be successful in the elimination of posterior pelvic tilt, reduction in sacral pressures, and minimize the risk of pressure-related skin breakdown. Photo 3: Ideal lower-extremity positioning is achievable via pressure mapping. Femurs that are not positioned parallel to the seating surface, as seen above, may result in dangerous pressure to the distal femur, resulting in breakdown to the posterior thigh. Photo 4: Fluctuations in seat to back angle and pelvic positioning can result in wide variances in pressure. Pressure mapping offers new insight and eliminates the guessing game formerly associated with seating and positioning.[/sidebar]
Kyphosis Intervention
Consider a client who presents with a flexible kyphotic presentation. Kyphosis, defined as an exaggeration of the normal posterior curve of the thoracic spine, is often seen in conjunction with posterior pelvic tilt, a presentation where the top of the pelvis tilts posteriorly toward the seat back, resulting in a significant increase in bilateral ischial tuberosity pressures, frequently resulting in skin compromise or breakdown. This posterior pelvic tilt often is unseen to the naked eye, and the severity and potential for damage that exists can be fierce and often life-changing.
Many options exist for the clinician to intervene and neutralize this flexible kyphotic position, thus rectifying the resulting posterior pelvic tilt. The rehab marketplace offers a line of anterior chest supports that help prevent the shoulder protraction seen with kyphosis, neutralize the trunk, and stabilize the torso. When used in conjunction with a two- or four-point pelvic belt or the more aggressive hip grip for greater pelvic stabilization, flexible kyphosis and subsequently posterior pelvic tilt can effectively be neutralized. Confirmation of this improvement in positioning can be achieved via use of one of many pressure mapping systems currently on the market.
Through the use of a baseline reading of bilateral ischial tuberosity pressures, which with significant kyphosis are anticipated to be higher than average and beyond an acceptable threshold, the clinician may confirm improved readings following the implementation of the above-noted interventions. As evidenced in the middle photo (see below), increased pressures to the bilateral ischial tuberosities and a sacral convergence of pressure suggest posterior pelvic tilt and kyphosis. In the bottom photo (see below), following intervention to neutralize kyphosis and achieve ideal pelvic positioning, ischial pressures are reduced and sacral convergence has been eliminated.
[sidebar float=”center” width=”250″]
Top: Pelvic obliquity, often not visible to the naked eye, but easily identifiable via the use of pressure mapping, can frequently be a silent culprit of pressure-related wounds. Middle: Kyphosis and postrior pelvic tilt, as evidenced here, not only increases the pressure under the bilateral ischial tuberosities, but also promotes sacral convergence of pressure, posing a significant risk to the sacral region. Bottom: Following intervention to neutralization kyphosis and achieve ideal pelvic positioning results in improved ischial pressures and reduced sacral convergence.[/sidebar]
Pelvic Obliquity Intervention
Pressure mapping is also a successful tool to confirm the success of intervention to neutralize pelvic obliquity. Pelvic obliquity is present when one iliac crest of the pelvis is not equal to the opposing side. A spectrum of pelvic obliquity exists ranging from correctable (also known as flexible) to non-correctable (otherwise known as fixed). Pelvic obliquities, which may not be visible to the naked eye, or are otherwise unidentifiable, are easily visualized via the use of pressure mapping (top photo, above), as is the notable increase in pressure at the site of the ischial tuberosity under the client’s low side of the pelvis. In order for pressure to be distributed evenly and threatening pressure wounds or ulcers to be circumvented, pressure must be evenly distributed, and this is instantly identifiable via mapping.
When evaluating a client with a pelvic oblique presentation, in order to fully assess the flexibility of the asymmetry, place the client on a firm surface, such as a therapy mat, or in a home health situation, a solid chair. Slide a flat hand under the low side of the client and raise the hand up. In the event the low side of the pelvis rises toward a neutral iliac crest height, a correctable or flexible pelvic obliquity is present. However, when a hand is slid under the low side of the pelvis and raised, with no identifiable change in iliac crest height, a noncorrectable or fixed pelvic deformity is present. When attempting to raise the hand, if the clinician is unable to adjust the pelvis, or no mobility at the pelvis is detected, yet asymmetry remains, a noncorrectable pelvic obliquity is present.
Through the use of an adjustable pelvic height cushion, the clinician may build the cushion height up under the low side of the flexible pelvis, or lower the cushion height under the high side of the pelvis in the case of a fixed or non-correctable deformity, thus neutralizing the pelvis and equalizing pressure. Multiple manufacturers offer adjustable-height cushion options which afford the clinician the capability to adjust pelvic height. Among these products are those designed to offer complete adjustability in individual pelvic height.
Skin Protection
Like many mobility device users who spend considerable time in a seated position, individuals affected by kyphosis who use mobility devices are at risk of developing pressure wounds. To help minimize this risk, therapists must make an informed choice when selecting cushioning materials. Cushions made of air, foam, gel, and combined mediums all offer specific benefits that can help preserve skin integrity.
Foam cushions typically require minimal maintenance, and some of the newest models are manufactured to have breathable properties. Foam cushions can be a relatively inexpensive option for a seating solution and do not carry a risk of leaking that is sometimes associated with air or gel cushions. Users may find, however, that foam materials can wear somewhat quickly and may tend to lose shape.
Cushions manufactured with polymer gels provide reduced shear while enabling movement of the bony prominences. They can offer a high level of comfort and are designed to provide extremely good pressure distribution. Polymer gel cushions sometimes are used in combination with a cushion that is foam-based. These types of cushions tend to be heavier than other types of materials, though, and may have the potential to “bottom out.”
Air cushions are an option that is inherently lightweight, designed to avoid “bottoming out,” and can minimize the buildup of heat and moisture. They also can be inflated to provide a high level of adjustability, with some models allowing quadrants of the cushion to be inflated separately. The maintenance required for air cushions may be greater than for other cushion types, however, and they may also be vulnerable to punctures or leaks.
For clients who require a combination of performance and protection, cushions are available that combine materials such as foam and air. These cushions can be highly customized to accommodate the specific shape and asymmetry of a mobility device user. Some manufacturers’ models feature air cushions with foam located internally that can help protect skin in the event of air loss.
Seat supports are an important seating accessory that can be used in tandem with a seat cushion to minimize uneven weight distribution that may occur with clients affected by kyphosis. The market currently offers models that have slip-resistant bottoms designed to prevent movement while in the mobility device, and helping to provide added comfort and fill gaps. Materials for seat supports should be easy to clean and resist moisture and mildew.
Accessorized for Comfort and Control
Therapists working with clients affected by kyphosis can also leverage seating components that will enhance the support and comfort those clients experience while using their mobility devices. Armrests, for example, can be used to pull away gravity from the arms and shoulders. These accessories are available in a range of styles, and they offer padding in various thicknesses.
Another important accessory for mobility device users are headrests, which can be particularly useful for mobility device users who need assistance in supporting their head. The latest headrests offer adjustability on multiple planes and are engineered to cup and support the user’s head. One type of headrest currently available provides drive controls as part of a head array that features multiple proximity sensors and swing-away options. The array is programmable and offers customizable pads designed to match a user’s seating system.
Seating solutions can also be further tailored to the mobility device user with the addition of abductors that separate a user’s knees and prevent adduction contractures. Likewise, knee adductors can be used to position the knees out of abduction.
Backrests, too, can be of particular importance when optimizing a seating solution for a user affected by kyphosis. For optimum fit, a backrest should spread the surface area over the user’s entire back, help to relieve pressure spots, offer a very high level of support, and help take weight off the spine. Models that can be easily adjusted to a variety of angles and can accommodate postural needs that change over time can offer good utility where kyphosis is a consideration.
Lower-Extremity Positioning Intervention
A frequent concern, which unfortunately is commonly missed upon assessment, is the position of the lower extremities in regard to the pelvis and trunk. Ideal lower-extremity presentation includes the femur in a parallel position to the seating surface, as well as the wheelchair seat depth typically stopping 2 inches short of the popliteal fossa (otherwise known as the back of the knee). If either of the above-noted positions is awry, significant and detrimental pressure could be present. When the femur and seating surface are not parallel, pressure will develop either at the location of the distal femur, in the event the knee is lower than the hip, or at the location of the ischial tuberosity if the knee is higher than the hip.
When incorporating pressure mapping into a client’s lower-extremity positioning assessment, the clinician should closely examine the distribution of femur pressure. In a well-positioned client, the higher pressure readings will present under the contact area with the pressures reducing as the end of the femur is reached (See Figure 3, page 28). When the knee is positioned above the hip, perhaps due to foot plates being positioned too high, or the seat to floor height being too short, the ischial pressures are increased and often, in more extreme presentations, the distal femur is not visualized on the pressure mapping system altogether. Often, this presentation is so minute, that it is not visible with the naked eye, especially when larger or comfortable pants (ie, pajama pants or sweatpants) are worn, but the ramifications of this angle are serious.
Prior to completing the lower-extremity positioning assessment, take a brief moment to perform a foot and heel analysis. Although traditionally used as a seating device, the pressure mapper of choice can quickly and easily be placed under the foot while positioned on the foot plate to verify proper weight distribution under the foot and heel. Correct pressure distribution at the foot and heel, especially with clients who may not always wear the proper footwear during wheelchair use, can play a significant role in protecting the heel and, in the case of ankle inversion, protect the lateral aspect of the foot as well. Simply place the pressure mapping sensor pad under the feet while on the foot plates to determine adequate positioning and pressure balance.
Pressure Mapping Options
Recent years have seen great expansion in the availability and variety of pressure mapping systems available. The technological advances and cost efficiency of those systems has provided the seating clinics of today with increased accessibility to pressure mapping, thus resulting in greatly improved outcomes, significant reduction in pressure-related wounds, and unprecedented client-equipment fit.
Resources for pressure mapping systems have grown more versatile than ever, and the expansion of these technologies set the stage for the introduction of low-cost, high-resolution systems, as well as the incorporation of pressure mapping technology into smart seating systems.
In recent years, thanks in part to the reduction in the cost of technology and continued advances in the field, some pressure mapping technology manufacturers are filling a niche where there is a need for low-cost and durable mapping systems designed for daily use. These manufacturers likewise are making other mapping applications available for sport use and gait analysis. Facilities and small clinics that previously were unable to attain pressure mapping are now finding several brands of mapping systems within reach; the result of new technologies offered by sources emerging in the marketplace.
While many clinicians are experienced in the art of ensuring proper wheelchair seating and positioning, many have yet to incorporate pressure mapping data into their assessment and fully explore the range and detail that pressure mapping can provide. With emerging technologies lowering cost as a barrier to entry, there are increasing opportunities for clinics to take advantage of the data pressure mapping systems can provide. Through the use of such systems and the incorporation of the subsequent data, today’s clinicians can more effectively confirm and support clinical decisions, as the use of a mapping device will tell the clinician far more than the naked eye would ever allow. RM
Kirsten N. Davin, OTDR/L, ATP, SMS, owns Escape Mobility Solutions LLC, Pleasant Plains, Ill, and specializes in wheelchair seating, positioning, and assistive technology provision. She conducts continuing education seminars and lectures nationwide. Davin also is a staff occupational therapist at Memorial Medical Center, Springfield, Ill, and on faculty at Rocky Mountain University of Health Professions, Provo, Utah. For more information, contact [email protected].










Author referenced “Recent years have seen great expansion in the availability and variety of pressure mapping systems available.”
…but failed to mention any? Or refrred to what to look for re: quallity?
I did not see any references. There should be some to validate the authors comments.
Thank you for your comment, Susan. The author did not provide any references, as I believe her clinical assertions are generally accepted throughout the profession. However, if you have questions about any specific points she made I would be happy to ask her to address them here. Please just let me know.
I would like the reference for providers of special cushions that address the pressure point mapping results.
I have ischael pain on my right hand side and use a Roho cushion that does not distribute my weight enough to avoid considerable pain. I know that I need to move to a cushion that is built especially for my need — but do not know of providers for these special cushions. Thank you very much, this is very important to me — and others. Gary Elsner