Photography by Richard T. Wardell Photography
Low back pain is a growing problem among America’s population. As the Baby Boom generation approaches its golden years, it is likely that health care dollars being spent on low back pain will rise dramatically. Current research demonstrates that there are numerous methods to decrease low back pain. When treating someone with this diagnosis, the therapist’s goal is to relieve the client’s pain and improve their function as much as possible. Once the client experiences relief from acute pain, they are educated in prevention of future occurrences of low back pain.
It is important to remember that chronic low back pain may not be relieved after a few physical therapy treatments. Most clients have been experiencing that pain for an extended period of time and complete pain relief may not be an attainable goal. However, increasing the patient’s function and decreasing their disability will increase their quality of life by enabling them to perform activities of daily living (ADLs) without assistance.
ASSESSING THE CLIENT
The first step of a physical therapy examination is to determine the client’s pain characteristics. A therapist will ask several questions related to the client’s pain including: Does the pain interfere with the client’s sleep? What movements make the pain better or worse? Did an initial event/movement trigger the pain? Is the client currently taking medications to ease the pain? These are just some questions that may be asked in order for the physical therapist to get a better understanding of the client’s pain. Other questions pertaining to the cardiopulmonary, integumentary, genitourinary, gastrointestinal, lymphatic, or endocrine systems may be asked to rule out any potential diagnoses not related to the musculoskeletal system. If the therapist suspects the presence of a condition that may be referring pain to the client’s low back, then the client will be referred to their primary care physician to be further evaluated.
The next step involves obtaining objective measurements to assess the client’s range of motion and strength. Manual Muscle Testing (MMT) is commonly performed to assess strength, and a goniometer or inclinometer is commonly used to assess range of motion in lumbar flexion, extension, rotation, and lateral flexion. Next, a movement screen will be performed. The client is first asked to lie on their back and bring both knees to their chest, slowly, 10 times. The PT will be assessing the client’s pain throughout the movement screen by asking them to quantify their pain on a 0 to 10 scale (0 is no pain and 10 is excruciating). The client is then asked to lie on their stomach and rise up on their elbows 10 times. Then, if they are able to tolerate it, the client is asked to rise up onto their hands with their elbows straight, 10 repetitions. The PT takes into account the findings from the examination, as well as the information gained from the subjective assessment, to develop a plan of care aimed to increase the client’s function.
A client’s work habits, hobbies, and ADLs are taken into account when an individualized plan of care is created. Based on the objective findings, a client is taught how to perform certain activities by avoiding movements that may increase pain. A strengthening program would be created to address weak muscles, and a stretching program would address any muscles that may be in spasm. Strengthening programs are developed to a client’s tolerance, generally starting with light weights and a few repetitions, then progressing to heavier weights with added repetitions.
MODALITIES TO DECREASE PAIN
Before active exercises can be initiated, the client’s pain must first be addressed. This is usually done through the use of modalities, a beneficial adjunct to any plan of care; however, they should not be the focus of treatment. The goal of using modalities is to decrease the client’s pain and to promote healing. Cold and hot therapies are commonly used to relieve the client’s acute pain at the start or end of treatment. They are traditionally the oldest and most popular modalities for pain relief and inflammation. Generally, ice or cold packs work best on recent injuries, and heat is better for long-term chronic pain. Both can be used in clinical and home settings.

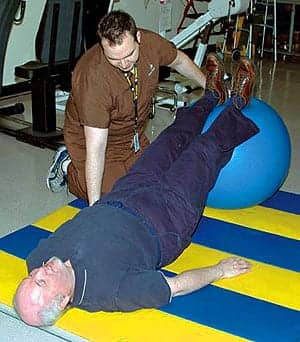
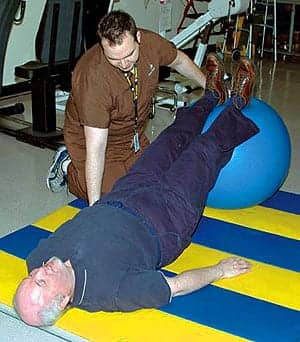
Author Stephen Merchant, DPT, employs muscle energy techniques on his client.
Another early modality to use on patients with acute and postoperative back pain is CPM (continuous passive motion), which gently activates the spine to help improve flexibility. The patient lies on a treatment table, which is set to incrementally move the patient for their comfort or tolerance.
Acute and chronic pain also can be addressed with the use of transcutaneous electrical nerve stimulation (TENS), which is often used in association with cold or hot therapies. TENS delivers a low dosage of electricity (in milliamps) to the affected area, creating pain relief via the gate theory. This theory works on the premise that painful signals are interrupted at the level of the spinal cord by pleasant non-pain-producing signals. In addition, the application of biofeedback can help break the cycle of tension and pain following injury. Biofeedback works as electrodes on the skin monitor bodily processes (that usually occur involuntarily), such as blood pressure, muscle tension, and skin temperature.
For noninvasive pain relief, iontophoresis uses low-dose electrical current to get water-soluble drugs through the skin. This method can provide therapeutic benefits with low side effects. (Studies have shown decreased pain in patients after they were treated via iontophoresis with dexamethasone.) Also, low-level laser can help with relief of back pain and muscle strain. Cold laser can be effective in relieving this pain, while being neither invasive nor addicting.
Topical gels and creams also may provide temporary pain relief by use of the gate theory. Topical gels/creams containing menthol will provide a cooling sensation as well as short-term relief for minor aches and pains. It is important to follow the label’s directions when using topical gels and creams to ensure proper use as well as safety. Additionally, therapists use topically applied products as a complement to such therapies as ultrasound, cryotherapy, TENS, and massage.
Muscle energy techniques are a type of osteopathic manipulative treatment used in osteopathic medicine and physical therapy. These treatments are not considered to be mobilizations or manipulations due to the fact that the client is providing the corrective force instead of the therapist. The goal of these techniques is to allow the body to assume a correct, natural position without muscle interference. Once the natural position is attained, the client is likely to experience a decrease in pain with an increased range of motion. Muscle energy is a direct and active technique in that a restrictive barrier is engaged and the client is encouraged to participate to their fullest potential in order to obtain a maximal effect. Several techniques exist that may be used in order for the body to assume its natural anatomical position. Research has shown that muscle energy techniques are beneficial in decreasing disability and improving function in patients experiencing low back pain. Once the client has achieved gains in their posture secondary to the use of muscle energy techniques, it is important for them to be educated regarding maintaining the proper posture achieved during all ADLs, as well as working activities.
STRENGTHENING AND HOME EXERCISE PROGRAMS
Core muscle strengthening and conditioning is imperative when treating back pain and can be accomplished by creating an individualized regimen of exercises using therapy bands, balls, and free weights, which can be overseen by the therapist in the clinic setting, or accomplished by the patient as part of a home exercise program.
Home exercise programs are an important element in an individualized plan of care for a client. These programs should help the client make gains in strength and endurance, as well as prevent any future occurrences of low back pain. Most home programs list seven to 10 exercises, which can be performed three to five times per day once the patient is discharged. Education regarding proper posture while sitting and standing, proper lifting techniques, as well as proper techniques during ADLs should be stressed when the home exercise program is given to the client. This education will significantly help in the prevention of low back pain.
Stephen Merchant, DPT, is a physical therapist at Banner Good Samaritan Rehabilitation Institute, Phoenix. For more information, contact .