Studies show that the majority of women who suffer from incontinence are too ashamed or embarrassed to talk about their symptoms with their partners or doctors.
However, no matter how bleak this situation may seem, there is hope and there are a number of treatments and methods to treat incontinence such as behavioral modification practices, exercises, biofeedback, physical therapy devices, diet, and pharmacology that can free a woman of the burden of one of the four types of incontinence she may be suffering from such as stress, urgency (commonly referred to as overactive bladder), mixed incontinence, and overflow.
In order to properly treat incontinence, it is important to discern which of the four types of incontinence the patient is suffering from. According to the National Association For Continence or NAFC (www.nafc.org), stress incontinence, a problem that commonly affects women, occurs when the pelvic muscles have been damaged, causing the bladder to leak during exercise, coughing, sneezing, laughing, or any type of body movement that puts pressure on the bladder.
AMONG THE CONDITIONS
Urge incontinence or overactive bladder is the urgent need to pass urine and the inability to get to the toilet on time. This occurs when nerve passages along the pathway from the bladder to the brain are damaged, causing a sudden bladder contraction that cannot be consciously inhibited. Stroke, dementia, Alzheimer’s disease, and multiple sclerosis (MS) can all cause urge incontinence.
Mixed incontinence occurs when symptoms of both stress and urge types of incontinence are present. Symptoms of one type of incontinence may be more severe than the other.
Overflow or chronic retention of urine incontinence refers to leakage that occurs when the quantity of urine produced exceeds the bladder’s holding capacity. It can result from diabetes, pelvic trauma, extensive pelvic surgery, pelvic organ prolapse in women, injuries to the spinal cord, shingles, MS, or polio.
Fecal incontinence is inability to control the passage or loss of gas, liquid, and/or solid stool (ranging from the loss of only a small amount of liquid waste, to an entire solid bowel movement).
BEHAVIORAL TECHNIQUES
According to the NAFC, some behavioral techniques can be used to treat incontinence such as scheduled toileting, bladder retraining, pelvic muscle rehabilitation, pharmacology, or surgery.
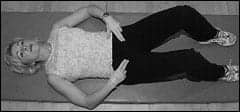 |
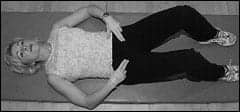
| Pelvic muscle exercise can be used alone or with pelvic floor stimulation, biofeedback, vaginal weight training, and/or magnetic therapy. |
Scheduled toileting is when the caregiver prompts the incontinent patient to void the bladder every 2 to 4 hours. The goal is simply to keep the patient dry, and this therapy is frequently recommended for frail elderly, bedridden, or Alzheimer’s patients.
Bladder retraining involves scheduled toileting, but the length of time between bathroom trips is gradually increased. This therapy trains the bladder to delay voiding for larger time intervals and has been proven effective in treating urge and mixed incontinence.
Pelvic muscle rehabilitation is a technique that involves pelvic muscle exercises (PME). PME may be used alone or in conjunction with biofeedback therapy, vaginal weight training, pelvic floor stimulation, and magnetic therapy.
 |
| Photos courtesy of Caitlin Costello’s Women’s Health Foundation |
Physicians can also prescribe medications to help control incontinence, and sometimes they will take a person off a drug that is causing or contributing to incontinence.
Surgical treatment should be performed only after receiving a thorough diagnosis from a health care professional. All appropriate nonsurgical treatments should be tried before deciding on surgery.
According to Missy Lavender, executive director and founder of the Women’s Health Foundation (www.womenshealthfoundation.org), the person should be aware of what they are eating and drinking. Diet sodas, caffeine, carbonation, artificial sweeteners, tomatoes, spicy foods, and certain medications can all irritate the bladder.
“We suggest women keep a bladder diary for 3 days and write down what they are eating and what and how much they are drinking and then start to look for a pattern,” Lavender says. “An average woman should be able to last 3 to 4 hours during the day before using the bathroom,” says Lavender.
Another behavioral trigger for stress incontinence is constipation, says Lavender.
“If a woman is chronically constipated, then she is straining so she needs to look at her diet and fiber intake,” she says.
“If a woman isn’t holding her urine long enough and if she gives the bladder the power to go when it wants to, then she can wind up bringing on symptoms of urge and frequency,” adds Lavender. “It’s important to hold it long enough for the bladder to be full.”
EXERCISES
The Women’s Health Foundation offers a fitness and educational program called Total Control. According to Lavender, not only does a woman need to do the right exercises but there are also things she needs to know in order to make necessary changes in her life.
“We really believe it’s the combination of exercises and education that makes the difference and we are proving this in clinical research. We know that our program, for example, has specific benefits,” adds Lavender
The Total Control Program teaches women proper pelvic floor exercise techniques, which can also be seen on the organization’s Web site at www.totalcontrolprogram.com as well as in its recently published book, You Go Girl, But Only When You Want To, and newly released DVD based on the pelvic pyramid called Total Control Workout: Be Fit, Be Sexy, Be In Control.
BIOFEEDBACK
Biofeedback is a group of techniques that use various sensors to detect muscular activity and present them in a way so that the patient becomes aware of whether she is producing the desired effect.
 |
 |
| Graphs mark the progress of biofeedback treatment for incontinence. | |
Biofeedback is an extremely useful tool for assisting women with learning how to do pelvic floor exercises, according to Lawrence Klein, PhD, vice president and cofounder of a Montreal, Quebec, Canada-based biofeedback and psychophysiological instrument manufacturer.
“Before surgery and drugs can be looked at, behavioral techniques such as biofeedback should be used for two reasons. The first being that it’s less expensive to treat the patients with biofeedback rather than surgery or using drugs on a continuing basis,” Klein says. “The second reason is quality of life. It’s a lot nicer to just do your pelvic floor muscle exercises than get injected with collagen or other invasive features, which are just a Band-Aid and do not provide long-term solutions,” he adds.
Klein compares learning how to do pelvic floor exercises without biofeedback to tossing darts with the lights off.
“Very often the patient will tighten the wrong muscle and biofeedback helps to isolate the correct muscle. Think of it as shooting darts with the lights off,” says Klein. “If you turn the lights on, it’s a lot easier to hit the target. Once patients know how to do the exercises properly, they take their [devices] home with them. Studies have suggested that there is a biofeedback success rate of more than 85%,” Klein adds.
Patricia Jenkyns, PT, Women’s Health Physical Therapy at Brigham and Women’s Hospital, Boston, says that through biofeedback, a woman is literally able to see if she is moving her muscles correctly and also learn where her pelvic floor muscles are by watching the electrical activity of her muscles on a computer screen.
“The one that we use is EMG (electromyographic), and you can see the electrical energy. It’s excellent to know that patients can really see when they are holding a lot of tension in their pelvic floor and they can learn how to relax the pelvic floor muscles by watching the screen,” says Jenkyns.
“I use biofeedback with most of my patients at different stages of their therapy. It’s a tool to help you see your body working, and I would say that most of my patients find biofeedback to be extremely helpful with learning how to contract and relax their pelvic floor muscles,” Jenkyns says.
PESSARIES
Orthotic dish or ring devices called pessaries are very useful for incontinence, according to Lavender, and they are often used for women who are postpartum or between babies and who are not candidates for surgery.
Very often women experience incontinence as a result of childbirth. During the delivery, the support structures are damaged and the pelvic floor and uterus start to drop.
 |
| Surface electromyography (or SEMG) and electrodes are applied in self-training of pelvic floor muscles with prescribed exercises, using either vaginal (shown), rectal, or surface sensors. |
“A pessary dish that looks like a thick diaphragm is inserted at will and it supports the uterus while a little knob presses against the urethra,” Lavender adds. “The device can be inserted by a nurse practitioner or qualified PT, and it’s a continuum of care whenever it is needed. The support device can really change lives for the better,” says Lavender.
ELECTRICAL STIMULATION
According to NAFC, percutaneous tibial nerve stimulation (PTNS) involves the delivery of electrical stimulation to the sacral nerve via the tibial nerve, accessed at the ankle. Many patients have been known to respond to this treatment. The stimulator generates a specific kind of electrical impulse that is delivered to the patient through the lead set using a needle electrode placed near the ankle as an enter point; the stimulator’s impulses travel along the tibial nerve to the nerves in the spine that control pelvic floor function. The system is designed to treat urinary urgency, urinary frequency and urge incontinence, and symptoms associated with overactive bladder.
For patients with symptoms caused by overactive bladder, there is a treatment that allows the delivery of electrical stimulation to the sacral nerves, called sacral neuromodulation or sacral nerve stimulation. It has been shown to be successful in four out of five patients with urge incontinence and successful in two-thirds of patients with urgency-frequency.
In a present study reported in the March issue of Urology, Jerilyn M. Latini, MD, from the University of Michigan in Ann Arbor, and colleagues assessed the outcomes of 41 patients with urinary urge incontinence who underwent a one- or two-stage implant procedure. During the follow-up periods of 4.5 months for two-staged implants and 12 months for one-staged implants, 90% of the patients experienced 50% or greater improvements in presenting symptoms and quality of life.
Unfortunately, many people change their lifestyles when their bladder habits begin to control their lives, which is a definite sign that a person should seek treatment right away if changes in their bladder or bowel habits are keeping them from doing what they want or need to do.
Gina Bernal is a contributing writer for Rehab Management. For more information, contact .