Nuket Curran, PT, DPT, prepares a flexible, wearable wrap that provides ice and heat therapy. The ability to wear ice can increase a patient’s level of participation in therapy. Likewise, the ability to wear thermal therapy to or from an appointment can save time for one-on-one treatment.
by Nuket Curran, PT, DPT Back pain is one diagnosis that leads many patients to seek physical therapy in a search of a “magic bullet” that will get rid of pain once and for all. Back pain prevalence is as high as 20.3% among all Americans, making it one of the leaders in disability in the nation.1 Physical therapy seeks to reduce pain and return the patient to optimal function. To do so, evidence-based practices must be used to reach appropriate rehab diagnoses and treatments. Adjunctive interventions including electrical modalities or passive applications are a common part of pain management in physical therapy treatment. But the question is, what is the most appropriate choice? Pain management has evolved rapidly. Evidence for many long-established interventions within physical therapy have not kept up with these changes. This puts the onus on the clinician to remain up to date in current pain management practices. Using the “SIN” of pain (severity, intensity and nature), the clinician can still determine what the pain might originate from. Some basic terms used to describe pain appear below in Table 1. 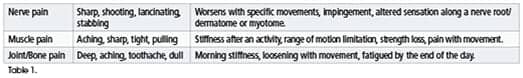
Choosing an Intervention
When choosing the appropriate intervention, the clinician considers many things in the process of formulating a rehab diagnosis of the patient using the International Classification of Functioning Disability and Health (ICF) model, for example. All of the data collected from the patient comes into play—history, social, economic, personal, and environmental—to help determine a holistic approach to the patient’s care. Some of the standard choices include the following modalities that appear in Table 2. 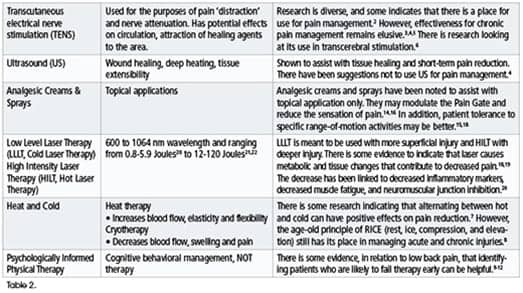
Psychological Factors
“Psychologically informed” physical therapy encompasses identification of patients with the likelihood of failure in therapy treatment due to psychological factors. The STarT Back tool was created13 to help clinicians identify “modifiable risk factors (biomedical, psychological, and social) for back pain disability.”13 Once patients are identified as high risk for long-term disability as a result of their back pain, clinicians are guided to seek either other healthcare providers with cognitive behavioral approaches or apply simple techniques with their patients. The tool itself is a nine-item questionnaire which asks the patient specific questions about pain and their perception of it. Where the Oswestry Disability Index measures function in relation to pain, the STarT Back tool asks pain attitude questions related to fear and anxiety from pain. It gives the clinician a “barometer” of patient pain perception as it relates to what they feel about their pain versus their actual pain.
Wearable Ice and Heat
When it comes to reimbursement and cost, these two items are nearly as prominent as pain management. The amount of reimbursement continues to decrease, while the cost to manage a business does not. Small physical therapy practices must balance these aspects and care of the patient. This includes considering the cost and value to the patient. To apply Aristotle’s thinking to healthcare, the best intervention chosen should be the right thing at the right time for the right reason. This is where adjunctive therapy devices can be useful when there is evidence to support them. For example, an adjustable, flexible wrap that provides wearable ice and heat therapy is available to the physical therapy market that incorporates thermal therapy with clothing to allow patient independence while being treated for back pain. A patient wearing this type of wrap can wear their thermal therapy to or from their treatment appointment, thus saving time for one-on-one physical therapy treatment. For patients affected by low to mid back pain who need ice or heat as part of their treatment, this type of wrap can be an effective solution for thermal therapy, time management, adjustable compression, and targeted vasoconstriction or vasodilation.
Good Care Lasts Forever
With the changes placed on physical therapists to provide efficient, cost-effective, evidence-based, high quality, and empathetic care, interventions that meet these needs are paramount. Clinicians must change “habits” and instead seek evidence-based practice and holistic approaches to determine a plan of care that meets the needs of the patient-consumer of healthcare. Old habits die hard, but good business practices and medical care lasts forever. RM Nuket Curran, PT, DPT, has been a physical therapist for 20 years and established her company, Fightin’ Fit Physical Therapy LLC, in 2016. She is an adjunct lecturer at Duquesne University and Utica College, and guest lectures for Chatham University. For more information, contact [email protected].
References
1. Clarke TC, Nahin RL, Barnes PM, Stussman BJ. Use of complementary health approaches for musculoskeletal pain disorders among adults: United States, 2012. Natl Health Stat Report. 2016;(98):1-12. 2. Santos M, Sato K, Santos E, Martins G, De Santana J. Evaluation of transcutaneous electrical stimulation (tens) in the treatment of an experimental model of neuropathic pain and its implications on functionality. J Pain. 2017;18(4):S88. https://doi.org/10.1016/j.jpain.2017.02.307 3. Spooner BM, Welch Bacon CE. The current evidence does not support the use of electrical stimulation to decrease pain and edema and improve function following a lateral ankle sprain: a critically appraised paper. Int J Athl Ther Train. 2017;22(4):1-5. https://doi.org/10.1123/ijatt.2016-0017 4. Wong JJ, Shearer HM, Mior S, et al. Are manual therapies, passive physical modalities, or acupuncture effective for the management of patients with whiplash-associated disorders or neck pain and associated disorders? An update of the Bone and Joint Decade Task Force on Neck Pain and Its Associated Disorders by the OPTIMa collaboration. Spine J. 2016:16(12);1598-1630. https://doi.org/10.1016/j.spinee.2015.08.024. Epub 2015 Dec 17. 5. Nelson R, Hayes D, Courier K. Clinical Electrotherapy. 3rd ed. Stamford, CT; Appleton & Lange; 1999. 6. Hazime F, Baptista A, Freitas D, et al. Treating low back pain with combined cerebral and peripheral electrical stimulation: A randomized, double-blind, factorial clinical trial. Eur J Pain. 2017;21(7):1132-1143. https://doi.org/10.1002/ejp.1037 7. Arankalle D, Wardle J, Nair PM. Alternate hot and cold application in the management of heel pain: A pilot study. Foot. 2016;2925-28. https://doi.org/10.1016/j.foot.2016.09.007 8. Teixeira E, Duarte J. Skeletal muscle loading changes its regenerative capacity. Sports Med. 2016;46(6):783-792. https://doi.org/10.1007/s40279-015-0462-0 9. Harris A, Moe TF, Eriksen HR, et al. Brief intervention, physical exercise and cognitive behavioural group therapy for patients with chronic low back pain (The CINS trial). Eur Journal Pain. 2017;21(8):1397-1407. https://doi.org/10.1002/ejp.1041 10. Wojciechowski M. Keeping pain out of the red zone. PT In Motion. 2017;9(6):24-31. 11. Campbell L, Kenardy J, Andersen T, McGregor L, Maujean A, Sterling M. Trauma-focused cognitive behaviour therapy and exercise for chronic whiplash: protocol of a randomised, controlled trial. J Physiother. 2015;61(I4):218. https://doi.org/10.1016/j.jphys.2015.07.003. Accessed October 17, 2017. 12. DeSantana JM, Walsh DM, Vance C, Rakel BA, Sluka KA. Effectiveness of transcutaneous electrical nerve stimulation for treatment of hyperalgesia and pain. Curr Rheumatol Rep. 2008;10(6):492-499. 13. Keele University. (n.d). What is the STarT Back Tool? https://www.keele.ac.uk/sbst/startbacktool/. Accessed November 3, 2017. 14. Shadgan B, Pakravan A, Hoens A, Reid W. Subcutaneous and intramuscular hemodynamics and oxygenation after cold-spray application as monitored by near-infrared spectroscopy. J Athl Train. 2015;50(8):800–805. https://doi.org/10.4085/1062-6050-50.6.02 15. Long B, Miller K. Influence of topical analgesic cream on passive hip flexion range of motion, sensation of pressure, and temperature. Athletic Training & Sports Health Care. 2016;8(2):55-62. 16. Strauss S, Grothe S, Usichenko T, Neumann N, Byblow W, Lotze W. Inhibition of the primary sensorimotor cortex by topical anesthesia of the forearm in patients with complex regional pain syndrome. Pain. 2015;156(12):2556–2561 17. Dima R, Tieppo Francio V, Towery C, Davani S. Review of literature on low-level laser therapy benefits for nonpharmacological pain control in chronic pain and osteoarthritis. Altern Ther Health Med. 2017. pii: AT5647. [Epub ahead of print] 18. Vanin S. Pain management takes a patient focus. Rehab Management: The Interdisciplinary Journal of Rehabilitation [serial online]. 2018;31(1):34-39. 19. Choi H-W, Lee J, Lee S, et al. Effects of high intensity laser therapy on pain and function of patients with chronic back pain. J Phys Ther Sci. 2017;29(6):1079-1081. https://doi.org/10.1589/jpts.29.1079. 20. Chow R, Johnson M, Lopes-Martins R, Bjordal J. Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomised placebo or active-treatment controlled trials. Lancet. 2009;374:1897-1908. 21. Angelova A, Ilieva EM. Effectiveness of high intensity laser therapy for reduction of pain in knee osteoarthritis. Pain Res Manag. 2016;2016:9163618. https://doi.org/10.1155/2016/9163618 22. Cotler HB, Chow RT, Hamblin MR, Carroll J. The use of low level laser therapy (LLLT) For musculoskeletal pain. MOJ Orthop Rheumatol. 2015;2(5):00068. 23. Wikipedia. Low-level laser therapy. https://en.wikipedia.org/wiki/Low-level_laser_therapy Accessed April 11, 2018.