 |
| Cherilyn G.Murer, JD, CRA |
The Centers for Medicare and Medicaid Services (CMS) created the diagnosis-related grouping (DRG) system in 1983. The original system involved all patient discharges being assigned a DRG, which grouped clinical diagnoses according to the expected use of hospital resources.
Under the previous system, there were 538 CMS DRGs. The DRG was determined by a principal diagnosis and up to eight secondary diagnoses that indicated comorbidities and complications. Additionally, DRGs were assigned a relative weight that reflected the average relative costliness of cases in that group compared with the costliness for the average Medicare patient (1.0).
In 2006, CMS announced a proposal that would implement the first significant changes of payment and policies for acute care hospital services to inpatients in more than 20 years. The proposed changes, according to CMS, reflected recommendations from the Medicare Payment Advisory Commission (MedPAC), and responded to some Congressional concerns that the existing system may create incentives for certain hospitals to “cherry pick” more profitable cases.
Additionally, CMS commented that the hospital payment reforms would mean that payments for hospital inpatient services will more accurately reflect the costs of providing the services. CMS’s goal was to take key steps to make payments equitable to providers and to assure beneficiary access to services in the most appropriate setting.
TRANSITION TO SEVERITY-BASED DRG SYSTEM
In August 2007, CMS finalized this proposal and CMS Acting Deputy Administrator Herb Kuhn states that Medicare payments for inpatient services “will be more accurate and better reflect the severity of the patient’s condition. “CMS says it adopted severity-based DRGs to prevent abuses under the current system.
The replacement of the old DRG (CMS-DRG) system, which was relatively stable since its 1983 inception, means that hospitals and, in particular, physicians and HIM, coding, and quality improvement departments must carefully work within the new system to ensure accurate reimbursement.
Effective for discharges after October 1, 2007, the new severity-based DRG System applies. The rule creates 745 new severity-adjusted diagnosis-related groups to replace the current 538 DRGs. The 745 Medicare severity-based DRGs (MS-DRGs) are divided into three severity levels: MCC, CC, and Non-CC. The familiar complication and comorbidity (CC) classification has been expanded to include CCs and major CCs (MCCs), which are conditions that require double the additional resources of a normal CC.
Additionally, the list of complications and comorbidities has changed. Some complications and comorbidities have been deleted and several have been added. Examples of secondary diagnoses that were previously considered complications and comorbidities that have been removed from the list include the following: unspecified congestive heart failure or other heart failure, unspecified chronic airway obstruction (COPD), and renal dialysis status.
 |
While several complications and comorbidities have been removed from the list, several complications and comorbidities have been added. Some of the more useful additions include: hemiplegia, any type, affecting any side; acute rheumatic pericarditis, endocarditis, myocarditis, other and unspecified acute rheumatic heart disease; all GI ulcers; chronic and unspecified osteomyelitis (all sites); and body mass index (BMI), less than 19 or 40 and over, adult. Ultimately, the introduction of new complications and comorbidities provides a new opportunity for appropriate reimbursement, subject to precise physician documentation and accurate coding.
The new system should not necessarily change the way coders assign codes, but coders must be more cognizant of capturing every complication/comorbidity (CC) and more specific diagnoses. The good news with the new MS-DRG system is that coders will still report ICD-9-CM codes using the same principal/secondary diagnosis and procedure coding conventions as before. Other changes are relatively minor.
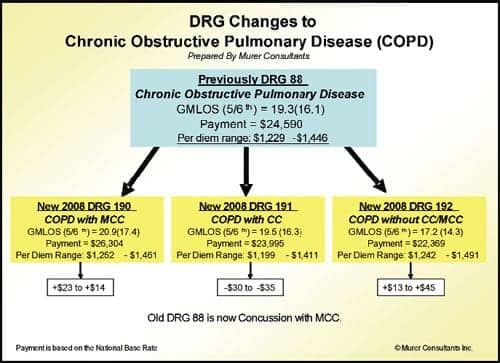
The base DRGs, for all practical purposes, remain the same, although they will have different numbers and there is some consolidation. It also takes only one CC or one MCC to change a DRG. CMS also restored five CCs and four MCCs that were previously deleted, including acute blood loss anemia (285.1) and trifascicular block (426.54), among others. Coma (780.01) is now an MCC. The diagrams are illustrations of how the new system changes the DRG numbering system and rates.
The bad news is that CMS is implementing a corresponding 4.8% payment cut over a 3-year period, including a 1.2% reduction for FY 2008 and proposed 1.8% reductions for FYs 2009 and 2010. This reduction is to offset the improved documentation and coding (and therefore payment) CMS believes providers will adopt, based on past data. CMS has stated that substantial evidence supports the conclusion that the adoption of new payment systems leads to an increase in aggregate payments without any corresponding growth in actual patient severity.
Medicare also will accept only the first nine diagnoses and six procedures on hospital bills, not the first 25 diagnoses allowed in electronic billing, which makes sequencing crucial. Therefore, it is important to note that an increased number of diagnoses reported on the UB-04 will not all be considered by CMS for billing purposes. Coders must appropriately and accurately sequence the most important diagnoses and procedures on the hospital bills.
CONCLUSION
The new severity-based DRG system should have a positive effect for hospitals with a more severe case mix index. However, this may cause problems for physicians because it will require them to give coders even more specific information than they do now. Since the new DRG system bases reimbursement on levels of severity, physicians must carefully document severe conditions or comorbidities in the patient chart in order to support assigning the new DRG. Therefore, now more than ever, it is imperative for physicians to ensure accurate and detailed documentation in patient charts.
The bottom line is that hospitals must implement clinical documentation improvement programs that engage both medical and coding staff to cooperatively document and report illness severity using ICD-9-CM terminology. Given the 1.2% documentation and coding adjustment, and the complete revision of the CC/MCC structure, hospitals that do not implement such a clinical documentation program may be left behind and face reduced reimbursement under the new DRG system.
 |
Cherilyn G.Murer, JD, CRA,is CEO and founder of the Murer Group, a legal-based health care management consulting firm in Joliet, Ill, specializing in strategic analysis and business development. Murer may be reached at (815)727-3355, or viewed on her Web site at www.murer.com.





