|
For decades, the ultrasound treatment modality has played a prominent role in pain management. In fact, 30 years ago, it was practically a given for every client to have the high- or low-frequency sound waves applied to affected tissue.
“You basically never would get out of a PT clinic without somebody hitting you with an ultrasound,” says John Garzione, DPT, AAPM, of Chenango Therapeutics, Norwich, NY, and president of the Pain Management Special Interest Group of the American Physical Therapy Association’s Section on Orthopedics.
Since that time, ultrasound has fallen from must-have status to being a popular choice for certain cases, such as soft-tissue injuries, and is generally part of a larger overall treatment plan. While evidence-based practice has not shown the definitive need for ultrasound, PTs still find that ultrasound can be clinically beneficial for alleviating certain conditions, particularly for promoting muscle relaxation and pain reduction.
PREPARING THE TREATMENT
Not all conditions are a good fit for the ultrasound modality, but others, such as tendinosis of the elbow or the foot, are perfect candidates. “We used to call them tendinitis, but we found that they’re not really inflammatory,” Garzione says. “It is a kind of tendon degeneration. Ultrasound has been shown in some of the literature to potentiate the inflammatory response.”
Because inflammation is generally the first sign of healing, potentiating inflammation is desirable for clients with tendinosis, making ultrasound a good option. “If you look at a tendinosis, you really want an inflammatory response to come back and kick in healing again,” Garzione says. “If an area is already inflamed, you certainly don’t want to potentiate the inflammatory response.”
Once the initial diagnostic exam has been performed, and ultrasound has been named the modality of choice, PTs must choose the appropriate dosages, treatment times, and frequencies. It all begins by examining the affected tissue itself. “We’ll look first at the tissue that we want to affect,” Garzione says. “Is it superficial, or is it deep? Do we want to heat the tissue, or do we want to just do the micro-massaging that ultrasound does in a pulsed wave?”
For deep structures that require heating, Garzione might apply a 1 MHz frequency, which penetrates and heats deeper tissue. In this scenario, dosage depends on how quickly the therapist wants to heat the tissue. To heat quickly, a higher dosage, such as 1.5 watts per square centimeter, is used.
It is also important to keep the size of the affected area in mind when choosing the sound head to be used during the treatment. Based on the size of the sound head, treatment time can be determined—for example, a larger area might require a 10-minute treatment. Generally, treatment times run between 5 and 15 minutes.
“There are some small sound heads,” Garzione says. “If you’re going to do a big area, you will be spending a lot more time. If the area you’re going to irradiate is probably three times the size of the sound head, then you’ll probably be on a 10-minute time frame.”
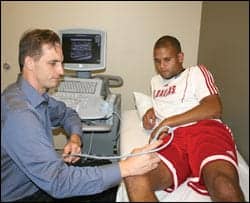 |
| A member of the FC Dallas professional soccer team receives ultrasound treatment. Many clients respond well to the application of therapeutic ultrasound, which is a favored treatment pain management. |
Once these decisions have been made, transmission gel is applied to the affected area, and the PT moves the sound head slowly over the area to be treated until the prescribed time is up. Continuously moving the sound head is important, as resting it on one area for too long could cause pain or damage, especially if the ultrasound is concentrated on the bone. “The ultrasound can go right to the bone and pull on the periosteum, which causes pain,” Garzione says.
There are different schools of thought on how many ultrasound treatment sessions are beneficial to clients. A long-held standard was that clients should have no more than 10 treatments—a number Garzione says was based on the study of a pig bone that started to show degeneration after 10 ultrasound treatments. “Some of the clinical research doesn’t support that as far as the exact number of 10,” he says. “So, as a rule of thumb, if it’s not effecting change or having a positive effect in three to four treatments, it isn’t going to work.”
For clients that get to the 10-treatment mark, Garzione works with the individual to determine whether the ultrasound modality is making a difference for them. “My questions would have to be, how much better are you?” he says. “How much better do you need to be? Is it the ultrasound that is helping, or some of the other procedures we’re doing?” After determining the answers to these questions, Garzione can better decide whether to continue with the ultrasound modality.
While the client’s verbal assessment of improvement counts for about 50% of the equation for Garzione, he also looks for objective clinical improvement. “When we do our examination, we’re always looking for objective signs, whether it be improved range of motion, less muscle spasm, more muscle strength, or decreased skin temperature,” he says.
Therapeutic ultrasound still has a strong role to play in pain management, and many clients respond well. However, PTs must also be prepared to walk away from it, if necessary. “The biggest advice, and what I tell my students, is that ultrasound can be an irritant,” Garzione says. “I’ll see four or five patients a week who have gone to other clinics where they’ve had ultrasound and they were in fact getting worse. The reason is because it was just randomly applied, and it was making people worse instead of better.”
PTs must make sure to constantly communicate with clients to find out how they feel after each treatment. If they feel terrible afterwards, Garzione says it is likely an adverse reaction to ultrasound and that the modality may not be for them.
UPDATED TECHNOLOGY
Today’s ultrasound models are sleeker than their ancestors, thanks in large part to the development of more compact computer technology. “You can get ultrasound units that you can combine with electrical stimulation, and portable units that you can carry with you,” Garzione says. The result is a unit that will not take up too much space in the practice.
For the most part, the ultrasound units are ready to apply when clients come into the practice. Cleaning the sound heads between clients is generally as easy as wiping off the gel from the sound head, then using an alcohol-based spray cleaner for sterilization. The sound heads come in a variety of sizes so that PTs can choose the one that best fits the size of the treatment area.
To learn more about ultrasound therapy, read “Penetrating Therapy” from our July 2006 issue.
Each year, the units should have a routine maintenance check to make sure there is no line leakage and the power level is where it should be. For the most part, maintenance is easy, but proper diligence is still required. “Once every couple of years, you may be sending a sound head or unit out for repairs,” Garzione says. “It’s not a high-maintenance modality, but then again, it’s not the lowest-maintenance modality that we have either.”
Some clients may be tempted by ultrasound units that they can purchase over the Internet to use at home, but Garzione cautions against this, as improper use could cause damage. An article he read several years ago recounted the story of a woman with arthritis who used a home ultrasound unit three to four times per day. “She was actually admitted into an emergency room with too much calcium in her blood because what she was doing was actually breaking down her bone,” he says.
To avoid putting his clients in a similar situation, he does not offer home ultrasound as an option. “I don’t let anybody take anything home that has the potential to do harm,” he says.
While interest in the applications of diagnostic ultrasound is growing in the physical therapy field, the traditional therapeutic ultrasound model will likely remain the same for the foreseeable future. “I’m not really sure we’re going to get into anything different in therapeutic unless maybe they start changing frequencies—instead of 3.3 MHz, maybe we’ll see somebody coming up to maybe 3.5 or 4 MHz for some other types of situations,” Garzione says.
Nancy Lorcan is a contributing writer for Rehab Management. For more information, contact .