by Adriaan Louw, PT, PhD, CSMT, and Jessie Podolak, PT, DPT, TPS
Patients attending physical therapy often ask the fundamental question: “What is wrong with me?”1 The answer to this question is far less complicated for someone with acute or immediate postoperative pain than it is for someone with chronic pain.1 Inevitably, clinicians using traditional models often answer “What is wrong with me?” by migrating to a biomedical explanation, focusing on faulty tissues as the source of any and all pain experiences.2
The biomedical model is very prevalent in physical therapy and is a sign that physical therapy curriculums need an update when it comes to pain science.2 While new theories are slowly gaining traction in the world of physical therapy, old theories still prevail. For example, in 1965 the Gate Control theory explained how an interaction of thin and large diameter nerve fibers can impede signal transmission in the dorsal horn of the spinal cord, changing processing and influencing an individual’s pain. This revolutionary theory was described in almost every textbook in the biological and medical sciences by the mid-1970s.3 More than 50 years later, the Gate Control theory is still used as the primary model to teach pain in physical therapy schools, despite the original author (Melzack) asking clinicians and scientists to expand their pain knowledge, moving beyond the Gate Control theory.3
With advances in brain scanning, neuro-immunology, neuroplasticity, and our understanding of psychosocial contributors, it is reasonable to question if the modern physical therapist is equipped to deal with the pain epidemic.4 What about hindsight? Well, for many years (and even now) when people in knee pain came to physical therapy and asked, “What is wrong with me?” we taught them everything we know about…the knee. Yet they are attending physical therapy due to pain!1 Would it not make more sense to teach them about pain? This “discovery” has led to the development of an emerging and exciting approach called Pain Neuroscience Education (PNE).5
Pain Neuroscience Education
PNE is an educational strategy primarily used by PTs that focuses on teaching patients about the neurobiological and neurophysiological processes involved in their pain experience.5 By teaching patients more about the biology and physiology of their pain experience, they develop a deeper understanding of pain, which has been shown to have significant clinical benefit. Current best-evidence related to PNE for musculoskeletal pain provides strong support for PNE to positively influence pain ratings, dysfunction, fear-avoidance, pain-catastrophization, limitations in movement, pain knowledge, and healthcare utilization.5,6
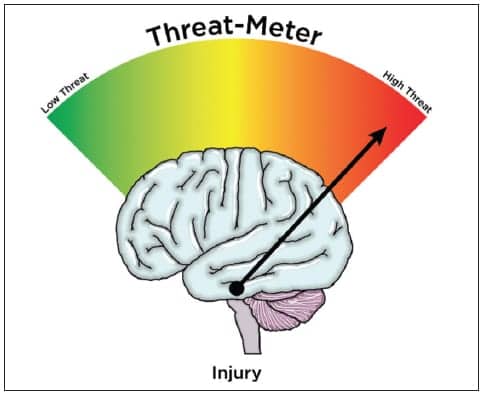
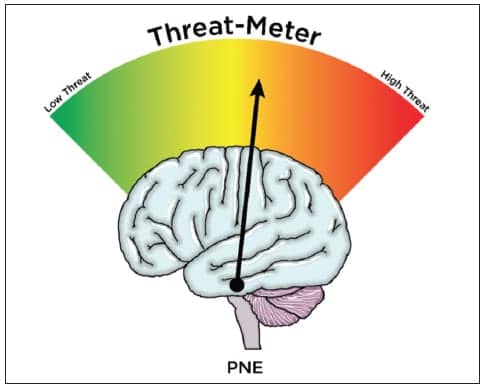
How and why does PNE work? The answer is likely complicated, but one area of interest pertains to the alteration of threat.4 It is now universally accepted that pain is produced by the brain based on the perception of threat. For example, when the brain receives information from the knee (nociception), it is processed by various areas of the brain (pain neuromatrix), mixed with adjacent neuronal circuits pertaining to memory, environmental issues, past experiences, social constructs, etc, ultimately allowing the brain to appraise the threat and make a decision.4,7 If a threat is perceived, pain is produced to protect. In this mode (facilitation), various physiological and biological processes are engaged to send more information to the brain (Figure 1).
It has been postulated that the unknowns surrounding “What’s wrong with me?” produce a high level of threat, especially when it mixes with failed treatments, different explanations of pain, concerns about work, finances, etc, as well as the various provocative words often used in physical therapy, including “torn, ripped, unstable, etc.”1,2,4 Teaching patients more about pain and alleviating many of the unknowns and fears associated with pain alters threat, which in turn alters the pain experience. Many PNE studies have shown that PNE alters fear, fear-avoidance, and kinesiophobia, which has been correlated to decreases in pain, disability, and movement impairments (Figure 2).5,6 What makes PNE appealing to PTs is the fact that it has shown significant efficacy for people struggling with chronic pain. PNE, however, has also been shrouded in controversy, specifically in regards to its clinical application. With the emergence of PNE, including its growing popularity at regional, national, and international PT conferences, some have assumed PNE is a treatment for people in chronic pain only, and that PNE is an education-only approach. This could not be further from the truth.
PNE+
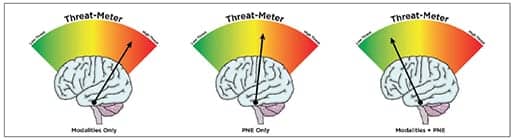
A common pitfall in research is the testing of a singular treatment technique. In a real clinical setting, patients often receive multimodal care that may include education, exercise, hands-on techniques, and modalities. It has been argued that clinical trials should be built on multimodal care to better represent real clinical practice. In regards to PNE, this is also the case. Two recent systematic reviews on PNE have shown that PNE is often delivered in such a multimodal format, versus an education-alone format.5,6 The reviews showed that PNE is often combined with manual therapy, exercise, modalities, etc. The most recent systematic review demonstrated that PNE, when combined with other commonly used physical therapy treatments, is far superior to PNE alone, when it comes to pain reduction for musculoskeletal pain.5
The PNE+ concept allows clinicians to utilize not only PNE, but to merge it with other treatments, which by itself may also alter the threat appraisal of the brain. In line with current evidence, it’s strongly suggested PNE be combined with active treatments, specifically exercise, and as a means to create independence on the patient’s part. Even though this statement is correct and in line with current best evidence, it has once again resulted in a major pendulum shift. In lieu of the aforementioned information, therapists have forgotten many of the proven treatments for pain management that may also help people who are suffering, including therapeutic modalities.
Therapeutic Modalities
With the emergence of “exciting” research such as clinical prediction rules, spinal manipulation, PNE, and now dry needling, PTs may have forgotten or started looking down on therapeutic modalities. Have we forgotten how modalities can alter a pain experience? Here’s a quick and powerful reminder:
• C-fiber activity is closely linked to persistent pain by its persistent firing into the dorsal horn of the spinal cord as well as its increased release of pro-inflammatory chemicals, all associated with chronic pain. Cryotherapy has been shown to slow C-fiber activity down, thus decreasing the nociception being sent into the dorsal horn and ultimately decreasing the threat appraisal of the brain.8 Additionally, via its vasoactive properties, ice has been shown to decrease pro-inflammatory chemicals in injured and diseased tissues, which further decreases nociception.
• Electrical stimulation, including transcutaneous electrical stimulation (TENS), has been shown to be effective in altering pain experiences via Gate Control.9 By altering the amount and duration of peripheral input to the central nervous system, it alters information passed onto the brain and the threat appraisal of the brain. Apart from its “electrical” benefits, TENS should be seen as a means to facilitate self-efficacy by providing a patient with the means to help themselves with their pain and develop independence over time.
• Recent work by Australian researchers has shown that electrical stimulation may in fact result in meaningful changes in cortical maps in the motor cortex, which in turn alter a pain experience, motor control, and disability.10
Additionally, in line with modern pain science, we argue modalities should be seen as a significant option in the “plus” part of PNE+. By combining the various potential benefits of modalities with PNE, the combination may indeed be more powerful than PNE alone (Figure 3).
Conclusion
If pain is produced by the brain, based on perception of threat, clinicians should realize they’re in the business of altering threat. Threat appraisal can be altered top down (PNE), bottom up (modalities), or more powerfully top down while bottom up. One approach by itself is not the answer, and combining treatments for a collective benefit will always be the future of pain management. RM
Adriaan Louw, PT, PhD, CSMT, is author of Why You Hurt: Therapeutic Neuroscience Education System.
Jessie Podolak, PT, DPT, TPS, is owner of Phileo Health LLC. For more information, contact [email protected].
References
1. Gifford L. Aches and Pain. Cornwall: WordPress; 2014.
2. Nijs J, Roussel N, Paul van Wilgen C, Koke A, Smeets R. Thinking beyond muscles and joints: therapists’ and patients’ attitudes and beliefs regarding chronic musculoskeletal pain are key to applying effective treatment. Manual Therapy. Apr 2013;18(2):96-102.
3. Melzack R. From the gate to the neuromatrix. Pain. Aug 1999;Suppl 6:S121-126.
4. Moseley GL. Reconceptualising pain acording to modern pain sciences. Physical Therapy Reviews. 2007;12:169-178.
5. Louw A, Zimney K, Puentedura EJ, Diener I. The efficacy of pain neuroscience education on musculoskeletal pain: A systematic review of the literature. Physiother Theory Pract. Jun 28 2016:1-24.
6. Louw A, Diener I, Butler DS, Puentedura EJ. The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Arch Phys Med Rehabil. Dec 2011;92(12):2041-2056.
7. Moseley GL. A pain neuromatrix approach to patients with chronic pain. Manual Therapy. Aug 2003;8(3):130-140.
8. Herrera E, Sandoval MC, Camargo DM, Salvini TF. Motor and sensory nerve conduction are affected differently by ice pack, ice massage, and cold water immersion. Physical Therapy. Apr 2010;90(4):581-591.
9. Johnson MI, Paley CA, Howe TE, Sluka KA. Transcutaneous electrical nerve stimulation for acute pain. Cochrane Database Syst Rev. 2015(6):CD006142.
10. Andrews RK, Schabrun SM, Ridding MC, Galea MP, Hodges PW, Chipchase LS. The effect of electrical stimulation on corticospinal excitability is dependent on application duration: a same subject pre-post test design. J Neuroeng Rehabil. Jun 10 2013;10:51.