PHOTO CAPTION: The Timed Up and Go (TUG) test measures walking balance, and can therefore help determine a person’s fall risk.
How to meet patient needs with technology that provides accurate and objective examinations.
by Mike Studer, PT, DPT, MHS, NCS, CEEAA, CWT, CSST, FAPTA
Whether your practice can be described with service lines of pediatrics, geriatrics, neurology, orthopedics, or sports, many of your patients are working on improving their balance. Balance, be it sitting or standing, is arguably a greater commonality across all of these patient populations than walking in, as this skill (the capacity to achieve and maintain balance) is a requirement even for those that have not learned how to walk yet—and for those that may never walk again. To effectively treat balance, we must be able to measure it, though. Measurement can be difficult, expensive, impractical, inaccessible, or inaccurate. Practicality (expense) and objectivity are among the main considerations in building your best balance lab, the technology that puts measurement within reach, which can itself be out of reach for a program’s bottom line.
Scope of Practice and Versatility
When making a decision about technology to measure balance, it can be particularly important to begin with a consideration of the scope of your practice—whom do you need to serve? If you are staffed to serve persons with sport-related concussion through orthopedics, your needs can be quite different than if you are providing care for persons with Parkinson’s disease (PwPD) and those recovering from stroke.
Regarding versatility, one must consider the diagnosis range and two considerations of the “functional range.” Diagnostic range is consistent with the discussion above about the scope of practice, but considers not only what your “main” customer sector is, but also the total range of whom you are serving. Meaning, if you are primarily working in spine and extremity orthopedics, yet also see persons with a history of stroke, neuropathy, or have a small niche practice seeing people after concussion or with positional vertigo (BPPV), then your range is much greater than orthopedics alone.
Functional range considers the abilities of your patients and what expressions of balance you will need to test so that your ceiling and floor are “far enough apart” to capture the performance and improvements for all of the people that you need to treat, document, and advocate for. Functional range can consider practice site and acute care versus outpatient, giving consideration to the severities of impairment within the same diagnostic groups that you are most likely to encounter.
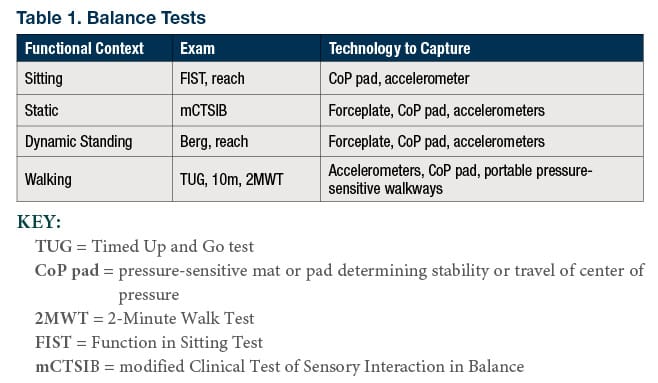
Functional range also considers the versatility of the suite of balance tests that you can operate, from static standing balance (mCTSIB), through dynamic standing balance (alternate step touch, Berg, functional reach, or limits of stability), or even into walking balance {Timed Up and Go (TUG); 10-meter walk test, 2-minute walk test}. Table 1 expands this conversation to suit your level of familiarity with balance tests.
Portability and the Value of Space
Some clinics and rehabilitation centers are blessed with significant endowments, affording spacious gyms, duplicated equipment, and dedicated testing examination or performance labs. Most do not have these luxuries. When decision-makers need to think about stewardship, considerations of portability favor equipment that can span different clinic spaces, various floors of a hospital, and programs within an acute rehabilitation unit (ARU) and skilled nursing facility (SNF). Related to these considerations is the increasing burden on home health providers to measure with objectivity. Here again, portability may reign.
No matter the cost and portability of an item, all equipment must be stored somewhere. That can mean dedicated square footage for a force plate, a dynamic posturography unit, or instrumented treadmill. Alternatively, a center of pressure mat, a collection of accelerometers, or even a roll-up walkway affords spaces to be repurposed quickly depending on the current needs.

Reliability and Interface
If the technology is not easily accessed or adopted, the expense, space, and function make essentially no difference. Large purchases that collect dust are nothing more than a transient public relations or marketing booster. Seeing equipment that is unused can be very disengaging for staff, causing well-intentioned long-term employees to wonder about how well their program is advancing with the times.
Purchasing decisions for balance treatment and examination technology should be relatively easy for the considerations covered so far. What functions must be tested? Walking, and both static and dynamic standing balance are the three main considerations. Examinations of standing balance (static and dynamic) are easy enough and unlikely to evolve (much) space when exams are being conducted. Economize your space well and purchase for the greatest good in considerations of program and patient benefit.
Ultimately, though, even the most economical purchase for space and budget is a poor choice if the clinicians do not adopt it as noted above, for any reason. The most common reasons for limited adoption are often hard to predict when decisions are informed by advertisements, sales representatives, or research studies. Problems of data storage, reliability, security, startup, speed, and the training required or relative intuitive nature of the operation are all salient in the ultimate reality of adoption.
In the world of technology, clinician adoption can be translated into considerations that may help readers ask the hard questions before writing any checks. Table 2 reflects some of the FMQs (frequently missed questions) that make or break a decision in the weeks and months after a purchase.
Table 2. Frequently Missed Questions
- Will this technology export data that integrates with our EMR?
2. What data do our customers need? (Fall risk score, normative data, incentives for wellness programming, accountability)
3. What is the most recent evidence?
4. What data helps to inform our practice best?
5. Are there two purchases that we could make for a similar expense in total, to cover a greater need in testing?
6. Did I consider what my staff want?
7, Are there other stakeholders that would appreciate the opportunity to provide input?
8. Do we have the space for this?
9. What is the opportunity cost? Meaning, what cannot be purchased due to space or expense, because of this decision?
10. Am I considering my entire program, or just a small sector? See question #9 again.
Is one of my options dually suited for testing and treatment?
The Almighty Data
Who is the most important consumer of your data at your clinic? Are you collecting data for your documentation, to meet state standards of practice or for reimbursement (authorization decisions, justification of skilled care)? No? OK, are you collecting data for marketing purposes—to show your referral sources and contract holders? No? OK, so you must be documenting to track your outcomes in an effort to study your treatment efficacy as a therapist or program? Certainly this is the most important, right?
Perhaps one of these is the most important reason for you to collect data, which may help to inform your purchase decision, as this dictates who needs to read it, how it can be displayed, and how it can be saved or sent. Considerations of electronic medical record (EMR) integration are salient here.
However, it is possible that none of these reasons to capture data is your main reason. You may need your new purchase to objectify balance in a manner that can engage your patients, providing them with an “independent arbitrator” that confirms their efforts in rehabilitation are leading to improvements.
Data presentation can be an easily overlooked consideration in your purchase. Don’t let this be the case in your efforts. Visual presentations of bar graphs with clear keys that guide a viewer, even if you are not there in person to interpret test results, may serve you best and most uniformly. Finally, with regard to data, we must consider the future. Is the database finite or cloud based? Will software performance be slowed by the size of the database in the near future?
Examination to Treatment
We know that the best balance lab cannot and should not stop at testing. That’s right…now you need to think about how to serve that population that you identified as having impaired balance, be they specific-to or a combination of pediatric, geriatric, of sport orientation, neurologic impairment, or orthopedic. A primary consideration here should be the opportunity to economize one or a few purchases that may be able to help your program both in examination and treatment. This could include using a pressure-sensitive mat for balance biofeedback, a portable pressure-sensitive walkway also for gait training, or even a consideration of an overhead track system with lift to afford higher level balance testing without risk and treatment of the same nature.
In today’s world of rehabilitation technology, the skies (lift systems) are literally the limit. Balance rehabilitation requires sophistication, accurate treatments that meet the identified need, and intensity. Your program may be able to accommodate gait trainers, supportive walkers, or even stair trainers pending population served with some consideration for your physical space and ceiling capacities.
Summary
Technology and budget aside, there are no substitutes for the combination of accurate and objective examinations that make sense to the patient, with intense rehabilitation that keeps the patient safe. With this combination, you have achieved patient engagement, minimized fear, and determined proper dosage. This is a “win” every time.
Investing in technology should always be a team decision. With advancements in balance technology, this must be considered a multidisciplinary decision. Sit down with your team and consider the table, your outcome measures, your clientele, and what your program needs. Your best balance lab will give you an opportunity to improve your practice outcomes (making more positive and real change in people’s lives); your efficiency (time spent to achieve an outcome, practitioner time spent in set-up/breakdown, reliably); your viability (stewardship of your finite resources of space, personnel, and money). If you are in the market for a purchase now or in the near future, you are in luck. The field of balance-related technology for examination and treatment is plentiful and improving in objectivity, functional scope, portability, and affordability. RM
Mike Studer, PT, DPT, MHS, NCS, CEEAA, CWT, CSST, FAPTA, is the owner of Northwest Rehabilitation Associates in Salem, Ore. For more information, contact [email protected].