 |
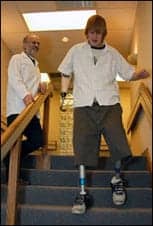
| With his new ankle for below-knee amputees, Theron Hogue can balance on hills and inclines. |
At no point in human history has there been a better time than now to lose a limb, so the argument could be made.
The wooden clichés found in the literature of Herman Melville are humbled before modern prosthetics: hydraulic wonders captained by microprocessors nestled within neat, composite metal frames. This advanced technology propels a team of orthopedic surgeons, physiatrists, prosthetists, and physical therapists, who usher amputees through the restorative process, and work in concert to achieve the best outcome circumstances allow.
The synergy between medicine and technology could hardly be better timed. The Centers for Disease Control and Prevention has labeled Type II diabetes an “epidemic” among an increasingly overweight and sedentary population—a population that seems ripe to develop the condition that is directly linked to 82% of the nation’s amputations.
The perfect storm may already have arrived.
BETTER, FASTER, STRONGER
If an uptick in amputations is imminent, the increased demand for prosthetic devices will likely be felt by firms such as Scott Sabolich Prosthetics and Research, Oklahoma City. The facility’s owner and clinical director, Scott Sabolich, CP, LP, has positioned the firm as a beta test site for certain component manufacturers, which affords Sabolich a glimpse at technology perched to revolutionize prosthetic function.
Two devices that have caught Sabolich’s eye are the Proprio Foot and iLimb Hand.
Sabolich says the new prosthetic foot improves on older models of mechanical feet that provided stability for an amputee but failed to allow adequate ankle motion, and precluded the wearer from pushing an automobile accelerator or being able to stand securely on an uneven surface.
“That’s something Proprio took into account, and they put something similar to a gyro on the device to keep the foot level on all planes,” Sabolich says. “When the prosthesis is swung through the gait cycle, it mechanically keeps the foot level, and the advantage that results is the wearer doesn’t stub their toe.
“A big, cool thing for an amputee,” Sabolich observes. “The only problem is Medicare has not deemed it medically necessary yet. It’s about a $14,000 ankle, so the majority of the population as private payors can’t get it.”
The iLimb Hand is a bionic device that entered development over the summer. The hand aims to leapfrog myoelectric devices engineered in the 1970s and revolutionize the function of prosthetic hands for upper extremity amputees.
“The old-style myoelectrics had provided one prehension pattern: the three-jaw-chuck,” Sabolich says, “so holding a ball or holding a bar was very difficult.”
The bionic prosthetic hand, Sabolich explains, is designed to master up to four of the five prehension patterns.
“Individual finger movement was once thought impossible, and we never really messed with it because we can barely get signals from the body to open and close the [prosthetic] hand,” Sabolich says. At the core of the hand’s technology are miniaturized motors that control each finger of the device, engineered to provide unprecedented dexterity.
A design revision that will downsize the palm currently has the new hand technology stopped short of a market rollout. Sabolich says he will begin fittings for several units that were ordered before the revised models become available. He expects the new devices to enter the market at roughly double the price of their myoelectric counterparts.
The high cost of prosthetic limbs is a reflection of the extensive research and development efforts to produce a product consumed by a very small market, according to Craig Gavras, executive director of Limbs for Life, a nonprofit organization that helps procure artificial limbs for those who cannot afford them.
Gavras says on average a below-knee prosthesis can cost $10,000 and above-knee models fetch around $20,000.
“Generally, people are very unaware of how much a prosthetic limb costs,” Gavras says. “A lot of people think you go to CVS Pharmacy and say, ‘I need a medium prosthetic,’ and they don’t realize the time and expense it takes to actually be fitted for a limb.
“It is not instant gratification,” Gavras says.
Kevin Carroll, MS, CP, vice president of orthotics for Hanger Orthopedic Group, points out the cost of owning a prosthetic limb—from $5,000 for a basic below-knee device to a $100,000 “dream machine” with a bionic knee—does not end with the purchase of the device.
“You have to protect it,” Carroll says, “and a protective cover ranges from $400 for a basic cover up to $8,000 for a cosmetic cover that is a mirror image of the other leg, which can take an artist a week of labor-intensive work to create.”
Only a fraction of amputees pursue the purchase of a high-end cosmetic covering, according to Carroll, and most choose to sheath their prosthetic foot in only a sock and shoe. Carroll notes the sale of cosmetic covers also reveals a gender gap among lower extremity prosthesis wearers. “Women by far are more concerned with how their prosthetics look, and are much more likely to be interested in a cosmetic cover, where men are more concerned about function: ‘What can I get out and do in this?’ ”
SOCKET TO ME
Though science continues to flirt with the process of attaching large prosthetics directly to bone, amputees who live in the world outside the laboratory rely on a prosthetist to create a socket that will join a prosthetic device to their residual limb. The importance of building a socket that fits well, Sabolich points out, trumps the value of even the most exotic performance features.
“You could put a solid gold foot on somebody, and it would have the value of a rock if it didn’t fit,” Sabolich says.
Of the 2 weeks an amputee spends at the Sabolich facility to procure a prosthetic limb, 95% of the time is dedicated to hand-molding plaster and fiberglass materials to sculpt in the bony musculature and pieces of the limb that form a negative mold of the residual limb.
“If a prosthesis doesn’t fit well and feel good, it won’t be put on and worn,” Sabolich says. “Then what good is it?”
Nearly half of Sabolich’s clinic is filled by amputees who come from out of state and are unable to be fit by their local prosthetist. Sabolich notes that often the fitting issues for these individuals stem less from poorly designed prostheses than from surgical technique. “The bones were left too short or too sharp, or there’ll be nerve problems, neuromas, or bone spurs.
“We have probably a 98% success rate, but of those successes, we’ll send 5% to 10% of those individuals back for revision surgery before we build them a prosthesis,” Sabolich says.
WORK WITH WHAT YOU HAVE
The man with no arms or legs was unusual that day among the 15 patients who came to see Diane Wilson, PT, at Walton Rehabilitation Outpatient Center, Augusta, Ga.
Wilson says the center attracts a higher than average number of amputees because of its proximity to a Veterans Affairs hospital, a regional burn center, and the Medical College of Georgia. Even so, individuals with bilateral amputations of upper and lower extremities rarely appear in Wilson’s clinical work, and road maps to guide their rehabilitation are even more scarce.
“There is not really a model for working with a case like this,” Wilson says, recalling the day the man arrived in a power wheelchair wearing “stubbies” and myoelectric prosthetic arms. Wilson engineered an aquatic program that used only the patient’s residual limbs. The bilateral AE/AK amputee wore a floatation belt at chest level that allowed him to perform the back stroke and breast stroke 45 minutes each day, 3 days per week, to build the heightened cardiovascular level prosthetics wearers need.
“I followed up with him this year, and he’s got his own business; he’s walking and he’s doing really well,” Wilson reports. “His attitude was, ‘I’m ready to get on with life and this is what I’ve got to work with.’
“So much of the outcome really depends on what’s inside them,” she adds.
Wilson says she has often drawn on her experience as a neurotherapist to fill the information gaps left by a vacuum of higher-level courses to educate therapists about amputee rehabilitation. Wilson says she used gait analysis skills she learned sleuthing lower-extremity muscular disparities of stroke and brain injury patients as a blueprint to work with lower-extremity amputees. Coupled with her understanding of the technology behind the prosthetics, the veteran therapist says she is able to treat an amputation almost as if it were a hemiplegic leg.
 |
 |
 |
| Kevin Carroll, MS, CP (far left), oversees his patients’ progress using their new prosthetic devices. | ||
Wilson and Sabolich agree that an increase in advanced learning opportunities for physical therapists who treat amputees would improve the current training prospects, which they both characterize as dismal.
“I’d take that a step further,” adds Sabolich, “and say, ‘Why is it so dismal for orthopedic surgeons?’ That’s where it starts.
“The limbs aren’t taken off right to begin with, then when they are, the patient is passed on to a prosthetist who may or may not know what they’re doing. Then they go to a PT who has no idea what they’re doing,” Sabolich says.
“There’s a need to increase PT training big time, and increase training for orthopedic surgeons on new parts and how long to leave the limbs so an amputee can use a prosthesis,” he adds.
Wilson suggests PTs build a core of knowledge of different types of prosthetics, which they can use to generalize from one device to another. She feels it is her responsibility to educate the patient about the process of getting a prosthesis and encourages amputees to consult peer groups for critical knowledge about components, device function, and how to communicate clearly with a prosthetist.
“Once a patient has that prosthesis, it takes an act of Congress to get it changed,” Wilson says. “Communicating the needs of your work, lifestyle, or important activities impacts the components that are put into the device.”
As amputees scrutinize the collection of technologies that will comprise the device they will live with for years, some discover newer may not mean better. Wilson says many upper-extremity amputees choose body-powered devices over myoelectric prosthetics. Lower-tech devices used for either extremity, she says, have shorter learning curves and fewer parts to break down while still providing good function. The bilateral AE/AK amputee Wilson treated found his myoelectric arms frustrating. The devices, Wilson remembers, were frequently “on the blink” and needed adjustments.
Wilson point out, however, that she considers prostheses built with the latest components to be “pretty intuitive.”
“Once prosthetic legs are put on, they do a great job of walking forward, and that’s 90% of what we’re teaching patients to do on them,” Wilson says. “They don’t back up very well and they don’t go sideways very well, but they walk forward.”
Carroll takes a different view.
“With the microprocessor knees, you can walk backwards all day long. And you can push and pull on things and drag things. It’s a learned behavior. The knees are programmed so they want to feel pressure on the heel. There is a resistance that comes into the knee mechanism and that’s what they’re pulling on,” Carroll offers. “It could be said that it’s strong enough to give you the strength to go in a walking back position. Side to side the same way, with the prosthetic feet they’re split. They have what we call inversion and eversion.”
Carroll and Wilson, however, both agree on how military personnel are reshaping the way the rehabilitation community thinks about outcomes.
“Military amputees have a mind-set where they’re just going to come, get on it, and get it done,” Wilson says.
Carroll admits he is impressed by what he has learned from the amputees.
“The soldiers don’t know fear. So they come to a flight of stairs and say, ‘OK, I’ll just walk down the way I always walk down.’ And you think to yourself, ‘How in the heck did he do that?’
“They are pushing the envelope,” Carroll says, “and we are learning from them. When I see a soldier accomplish something extraordinary, I think, ‘OK, a guy who lost his leg in a fire should be able to do the same as the soldier who lost his leg in combat.
“Hats off to them,” he adds.
Committed to “Get Them Up and Get Them Walking”
LIMBS FOR LIFE is a nonprofit organization based in Oklahoma City that provides a financial bridge for up to 3,000 amputees each year who cannot afford the cost of a prosthetic limb.
The foundation’s primary objective is to procure a prosthetic device for amputees that will get them up and walking as soon as possible, according to Craig Gavras, executive director of Limbs for Life.
“If a person gets into a wheelchair, sometimes they get to the point where they say, ‘This is my life, and there’s nothing I can do,’ ” Gavras explains. “Then when you try to get them into a prosthesis, it slows them down, and it’s almost a burden to them.”
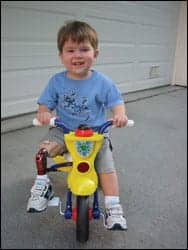 |
| Connor Karow demonstrates his prosthetic leg. |
Gavras says 70% or more of every dollar Limbs for Life receives from donors is directed to patient care, which steers the foundation away from pricey technology that would be expensive to maintain and would reduce the total number of devices the organization could provide. The roughly 700 amputees Limbs for Life assists annually are typically age 50 or older, are uninsured, and have lost a limb to diabetes. They are people too young for Medicare who lack the means to pay for the devices themselves.
Donated time and labor from prosthetics facilities and component donations from manufacturers enable Limbs for Life to procure prosthetic limbs at a fraction of their market cost. Physical therapy clinics nationwide also support the organization’s mission by donating an average of nine visits to amputees who receive a prosthesis from Limbs for Life.
The foundation creates a global impact with its efforts to collect and distribute donated limbs no longer used by their American owners. Gavras says the devices, which still function well, are shipped to clinics worldwide, where they are used by “people who can’t afford anything.”
Amputees, on average, can expect 5 years of service from a prosthetic until it must be replaced due to wear and tear, fluctuation in the wearer’s physiology, or reclassification of the wearer’s function level. Limbs for Life builds in an allowance for socket changes, which must be made as sockets wear out over time—more frequently among juvenile amputees. Less predictable, however, is whether an amputee will raise their function level at a rate that outpaces their prosthetic.
“If a prosthetist comes to us and says, ‘This individual started off at a function level 2 and they’re now at a function level 4,’ there is no question we’ll address that issue,” Gavras says. “A prosthesis that has fallen below a patient’s level of function will hinder that patient and hold them back.”
Though the cost of prosthetic limbs can be a shock to consumers, according to Gavras, he says the tremendous resources manufacturers devote to research efforts justify their market price. “Otto Bock spent an unbelievable amount of time and money doing research on the C-leg,” Gavras says, “and when you’ve got a small population that’s buying the product only once every 3 to 5 years, it takes a long time to get a return on your investment.
“The prosthesis is a very inexpensive medical tool that can get people up and walking and back to a normal life,” Gavras says. “And being able to walk by using a prosthetic is, in the long view, the healthier option to using a wheelchair.”
—FL
Frank Long is the associate editor of Rehab Management.





