
19-year-old Jaime Cavalleri, who suffered multiple brain stem CVAs, presents clinically with “locked in” syndrome and quadriparesis. He is independently mobile in a power wheelchair using a head array system.
The majority of children and adolescents participate in school and social activities without concern for mobility and seating. But for millions of youth with developmental disorders and physical disabilities, seating and mobility are barriers that can keep them from fully participating in school, and are a top priority for students, their families, and educators. On June 28, 2012, the US Supreme Court upheld the major tenets of the Affordable Care Act (ACA), legislation written to reform the health care system. As physical therapists, we are among the primary health professionals responsible for the physical health of children who have chronic severe disabilities such as developmental disability, acquired spinal cord injury (SCI), or brain injury. For these children, appropriate seating and wheeled mobility are foundations that can help ensure integration into school programs and peer activities.
SEATING AND THE CLASSROOM
While physically able-bodied children can sit almost anywhere—at desks, at tables, on the floor—special needs children frequently require seating that will provide additional stability (pelvis, trunk, and head), and encourage upright posture for alertness, interaction with peers, and comfort. Additional goals may include increased upper extremity function for activities of daily living, enhanced feeding ability, and various physiological health benefits.
When children have adequate trunk control to utilize a standard surface from a wheelchair, adjustable height desks and tables can meet their needs, with perhaps minimal rearrangement of furniture to increase access to an area. Numerous commercial seating options are available that address different levels of needs. Among these are corner chairs, which consist of a padded surface, converting a 90 degree “v” shaped back into a three-sided winged back, often with a lap and/or chest strap. This design provides support along the spine and trunk, affording trunk stability while allowing the child to freely use the arms and right the head. These seats are sometimes elevated off the floor, promoting thigh support and 90-90 sitting. Other corner seats can be placed on the floor, allowing full leg extension in a long sit manner, lengthening the hamstrings. Socially, this seating option enables children to participate in circle time floor activities on the same level with their peers.
A multitude of positioning chairs are available to accommodate the needs for upper and lower body support, trunk alignment, and repositioning and sometimes to provide a simple work space. Some basic designs simply provide back and lateral support in a rounded fashion, “hugging” the child to provide a sense of security. Other positioning chairs offer wider seat surfaces and bases of support to improve pelvic positioning and promote stable sitting.
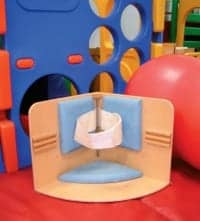
Corner chairs are designed with a “V” shaped solid back and a chest or lap strap, to provide trunk stability and free use of the arms.
The ability to tilt these chairs in a slightly forward manner shifts the pelvis into an anterior posture, activating weight bearing in the lower extremities and increasing extensor tone in the trunk. This activation of muscles is the result of the body’s reaction to gravity through the vestibular system and proprioceptors. This is frequently referred to as “active holding” or “co-activation.” It increases alertness as well as provides a “readiness” for activity of the head and arms.1 Tilting the chair posteriorly transfers the body’s pressure onto the back, and allows the child a rest period.
Other features of positioning or activity chairs include: trunk supports for lateral stability, headrests, lap trays (that may provide an inclined or level surface), lap/chest belts and abductor, and adductor wedges.
STANDING AT SCHOOL
For individuals who are seated in wheelchairs most of the day, periodic episodes of standing can prevent adverse effects of immobilization. Various standing devices are offered on the market. Prone, supine, and multiposition standers provide complete support and the level of upright or vertical is adjustable. Prone standers provide support on the chest and anterior body, offering a stretch to the hip flexors and a challenge to extend the head against gravity. The prone position also is gravity dependent, making functional tasks with the upper extremities more difficult. Supine standers support individuals on their back until they reach an upright position where they can balance their head control with gravity pulling it forward. Tables or trays can be placed in front of the standers to engage in activities. Sit to standers provide a seat or strap beneath the pelvis, which lifts the patient from a seated position to an upright standing position—or anywhere in between. These devices work well with larger, heavier youth who have good head and trunk control.
Dynamic or mobile standers provide all of the benefits of standing while also allowing the individual to be independently mobile, propelling the wheels with the upper extremities. Sometimes this is accomplished through a series of pulleys and wheels, and other models offer wheelchair-sized wheels in an anterior position. Dynamic standers require the individual to have good head and trunk control, as well as upper extremity strength.2

A client who requires total assist to come to stand can benefit from a sit to stander. This model also permits the child to be independently mobile and interact with others in a standing position.
The Rehabilitation Engineering & Assistive Technology Society of North America (RESNA) supports the incorporation of standing devices into school settings, with proper medical/professional supervision. Standing adds significant vertical access and functional reach. Since the seat surface moves to vertical, the vertical access is equal to the user’s seat depth. This allows a greater functional reach to access areas of the environment, such as sinks, countertops, and white boards in the classroom. The standing position places a mechanical stretch on the hip, knee, and plantar flexors, increasing passive range of motion to these joints and reducing the risk of contractures from sitting. Full upright standing relieves pressure 100% from the ischial tuberosities, diminishing the risk for pressure sores. Bone density loss may be decelerated in certain populations. Subjectively, many individuals report improvements with bowel and bladder function, as well as with circulation and respiration.3
Although funding sources rarely recognize the psychosocial benefits of standing devices, these advantages may be some of the most important. Eye-to-eye contact with peers increases socialization, emotional development, confidence, and self-esteem. Standing for the Pledge of Allegiance and participating in any activity meant to be performed upright creates a better sense of integration, with the disability becoming less visible, and individuals perceiving higher acceptance and reduced depression.3
When standers are incorporated into school programs for younger children, care should be taken to ensure a slightly abducted position to promote normal development of the femoral-acetabular joint and decrease the risk for hip dislocation.4
EXPANDED MOBILITY OPTIONS
Gait trainers also are used for independent mobility when impaired motor control and strength in the lower extremities are present. Differing levels of support can be provided at the upper extremities, trunk, and pelvis to decrease the demands on the weaker muscles utilized in walking. Gradual reductions in the supports will strengthen muscles and increase the child’s efforts of ambulation. The independent mobility encouraged at a young age contributes to cognitive growth with environmental exploration.5
Many of the concepts and equipment described previously are included in the Mobility Opportunities Via Education/Experience (MOVE) curriculum. MOVE is an activity-based program incorporated into many schools, designed to teach students functional motor skills (sitting, standing, and walking) needed for life skills in the home and community.6

Clients with weak neck and trunk control frequently require extensive seating systems for support. Tilt in space wheel-
chairs allow pressure relief and rest periods without changing the 90 degree hip position.
Powered mobility offers an alternative for independent locomotion when children cannot ambulate or self-propel a manual wheelchair. However, even when a child has limited ability to do either or both of these skills, it is often accomplished at a significantly increased energy cost. The pathological gait pattern associated with various disabilities often requires a greater amount of energy along with a less efficient velocity. Pediatric manual wheelchairs are often considerably heavier due to the weight of growth packages, seating systems, and transportation safety equipment. Axle plates are frequently placed more posteriorly to increase safety and stability; however, this wheel position is less ergonomic and can cause overuse injury to the shoulder girdle.7
Traditionally, use of a power wheelchair was viewed as a failure or giving up hope on interventions and strategies to normalize the movements of a child. The newer therapeutic model, Dynamic Systems Theory (DST), is more evidence-based and recognized today. DST considers the interactions between a person, task, and environment in regard to an individual’s motor development. It focuses on function and task accomplishment instead of normalized appearance as defined by traditional societal perceptions.8
It should be noted that mobility must be efficient, and not confused with exercise. Children with disabilities need cardiovascular exercise just as much as their able-bodied peers do. These concerns can be addressed through therapy and recreation.7
BENEFITS BEYOND THE BODY
Besides the physiological benefits (increased efficiency and energy conservation), the psychosocial and intellectual gains that mobility can provide are considerable. Mobility is associated with the acquisition of important cognitive and perceptual skills in normally developing children and among those who are mobility challenged. Improvements in cognition and perception are the result of children moving independently and facing a set of complex spatial problems, such as negotiating obstacles, not falling from stair ledges, and topographical orientation. Young children who do not have self-initiated mobility perform poorly on a wide range of developmental functional skills because these skills may not be relevant to their lives. Older children with limited mobility perform poorer than age appropriate peers with functional mobility when tested on map reading skills, remembering how to get to and from one place to another, and estimating the ability to negotiate tight spaces.9 Mobility impacts a child’s ability to learn and participate in school and society by increasing independence. Mobility allows the child to form a sense of identity and confidence. It reduces apathy and depression, improving self-esteem and confidence. It also helps to avoid learned helplessness. Learned helplessness leads to passive and dependent behaviors, as well as decreased curiosity and initiative. Providing efficient and functional mobility can reduce these risks in children who have impaired mobility.10

Seven-year-old Sthuart Reyes presents with C1 tetraplegia. He is age appropriately supervised with power wheelchair mobility using a pressure sensitive proportional joystick with his lips.
How early is a child ready for powered mobility? Chronological age and IQ are not good determinants of a child’s ability to operate a powered wheelchair. The Pediatric Powered Wheelchair Screening Test (PPWST) (Furumasu et al, 1999)11 can determine a cognitive developmental age. A child must demonstrate the ability to use an access method (joystick or switch) as well as exhibit cognitive, sensorimotor, and coping skills. Cognitive abilities include cause and effect, directional concepts, problem solving and spatial relationships, as well as judgment. Sensorimotor abilities include perception, processing, motor planning, and reaction time. Coping abilities include attention span, motivation, and persistence. Contraindications to powered mobility include uncorrectable compulsive self or other directed abusive behaviors.12
The training approach for powered wheelchair mobility is to incorporate the child’s own motivation and curiosity to spontaneously explore newly found movement through basic skills, then gradually introduce new tasks. The amount and type of training will vary with individuals based on their needs, deficits, motivation, and learning style. Generally, a child who demonstrates emerging skills and motivation to drive from one location to another, with limited cues and without running into obstacles, is ready for powered mobility.11 Other pediatric considerations to a powered wheelchair include power seat functions such as tilt, recline, seat elevator, and powered standing. RESNA does recommend early utilization of powered mobility for appropriate candidates as medically necessary to promote psycho-social development, reduce learned helplessness, and facilitate social and educational integration and independence.7
Following the Individuals with Disability Education Act of 2004, more than 6.5 million infants, toddlers, children, and adolescents receive early intervention, special education, and other related services in our schools.13 The students, families, educators, and therapists must collaborate thoroughly to ensure that all needs are evaluated and that goals are mutually set to guarantee stability, comfort, and mobility in order to maximize student learning and growth.
Deborah J. Levin, PT, received her Bachelor of Science degree in Physical Therapy from the State University of New York at Buffalo in 1990. She has been employed at Rancho Los Amigos National Rehabilitation Center in Downey, Calif, for 22 years, where she currently is a Physical Therapist II on the Pediatric and Adolescent Service. For more information, contact .
References
- Kangas KM. Seating for task performance. Rehab Management. June/July 2002.
- Warner M. The benefits of standing devices. www.rifton.com/resources/articles/fieldissues/benefitsofstanding.html
- RESNA Position Paper on the Application of Wheelchair Standing Devices. March 2007. www.ncbi.nlm.nih.gov/pubmed/19908680
- Macias LM. The effects of the standing programs with abduction for children with spastic diplegia. Pediatric Physical Therapy. 2005:1: 96.
- Bundonis J. Benefits of early mobility with an emphasis on gait training. www.rifton.com/adaptive-mobility-blog/benefits-of-early-mobility-with-an-emphasis-on-gait-training
- www.move-international.org
- RESNA Position Paper on the Application of Power Wheelchairs for Pediatric Users. www.ncbi.nlm.nih.gov/pubmed/20066888
- Wiart L, Darrah J. Changing philosophical perspectives on the management of children with physical disabilities: their effect on the use of powered mobility. Disabil Rehabil. 2002;24:492-498.
- Stanton D, Wilson PN, Foreman N. Effects of early mobility on shortcut performance in a simulated maze. Behavioural Brain Research. 2002;136:61-66.
- Butler C. Augmentative mobility. Why do it? Phys Med Rehabil Clin N Am. 1991;2(4):801-815.
- Furumasu J, Guerette, P, Tefft D. The development of a powered wheelchair mobility program for young children. Technology and Disability. 1996;5:41-48.
- Nilsson L, Nyberg P. Single-switch control versus powered wheelchair for training cause-effect relationships. Which to start with for individuals at an early developmental level? Technology and Disability. 1999;10:1-4.
- idea.ed.gov





