 |
| An example of a lower-extremity marker set used in a clinical gait analysis test. |
Gait, or individual walking style, is a complex task involving a delicate interplay of many body segments, requiring appropriate muscle activity at the appropriate time to maintain balance. Without precise coordination, walking can be awkward and unsafe. This is true for many patient populations with compromised joint motion due to static or dynamic factors such as contractures or spasticity.
The complexity of gait, particularly pathological gait, can make it difficult for clinicians to distinguish primary gait deviations from secondary, or compensatory, deviations. This is especially true when the primary means of diagnosis is patient observation alone. The technology available within clinical gait analysis (CGA) laboratories, however, is invaluable for identifying gait deviations that may be amenable to treatment intervention.
MOTION CAPTURE SYSTEM
The foundation of the CGA lab is the motion capture system, the same technology used by animators to create digital characters and video games. A common type of motion capture system uses high-speed, high-resolution video cameras trained on “markers” that are placed on specific body points. In many systems, the camera lens is surrounded by a strobe containing many LEDs. The light from the strobe reflects off the markers, which are covered with retroreflective tape, and is recaptured by the camera.
 |
| A high-speed, high-resolution video camera trains on these markers placed on specific body points. The camera lens is often surrounded by a strobe containing LEDs. |
At least two cameras must see each marker to recreate its three-dimensional location, so most CGA labs use at least six cameras to ensure redundant coverage. The cameras are synchronized to take photos simultaneously, allowing the individual images to be combined to calculate the three-dimensional location of any given marker at any given moment.
In clinical settings, the location of each marker is dictated by the part of the body being studied. For example, a different set of markers is used for a lower-extremity walking study than for an upper-extremity reaching test. To accurately capture movement, at least three reflective markers are placed on each body segment, preferably over bony landmarks. This allows the software to create a coordinate system for each segment of interest. For gait analysis, these might include the foot, the shank, the thigh, and the pelvis. With these coordinate systems, relative joint angles can be calculated for the ankle, knee, and hip. These relative joint angles allow CGA clinicians to see motion graphed in the sagittal, frontal, and transverse planes.
This three-dimensional assessment is a marked improvement over visual observation of patients walking in the hallway. For example, many children with cerebral palsy are described as walking with a “scissoring” gait pattern, characterized by hip adduction and legs that seem to cross over each other. The assumption may be that the hip adductors are overacting and causing hip adduction during the gait cycle.
Through three-dimensional gait analysis, however, it may be found that the apparent scissoring is actually a combination of hip internal rotation with hip and knee flexion. In this case, the human eye is fooled into seeing hip adduction that isn’t actually present. Consequently, treating the adductors would be inappropriate and unsuccessful for most patients. The primary issues may be other factors such as femoral anteversion (resulting in increased internal hip rotation) and hamstring contractures (contributing to increased knee flexion). Treatment of these clinical impairments may be more effective at decreasing the apparent scissoring.
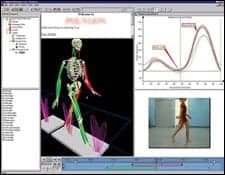 |
| The above program displays data gathered through the use of clinical gait analysis technology. Through the use of CGA technology, referring physicians have access to information that is otherwise not observable. |
ELECTROMYOGRAPHY
Another common component of clinical gait analysis labs is electromyography (EMG), the study of muscle activity. EMG provides information about which muscles are active when they should not be (therefore interfering with desired movement) and which are not active when they should be (therefore failing to achieve desired movement).
A treatment plan may be based, in part, on whether key muscles are acting appropriately. Thus, through CGA technology, referring physicians have access to information that is otherwise not observable.
FORCE PLATE
A third component of standard CGA laboratory technology is the force plate, a high-tech version of a bathroom scale. Typically embedded in the floor, the force plate records all forces when patients step on it. This data can be combined with kinematic information and the laws of physics to calculate joint kinetics (eg, forces and moments).
Though less intuitive than joint angles, net joint moments can tell a lot about how joint motion is managed by muscles and other tissues. Higher knee extensor moments, for example, may help explain or predict knee pain due to the added stresses on the joint. Joint kinetics may be the most valuable CGA data obtained during a typical test. Because it is a mathematically derived data type, a joint moment adds to the clinical picture of a client’s ambulation because it cannot be observed by watching a client walk.
OBJECTIVE, QUANTIFIABLE DATA
One of the most beneficial aspects of CGA is the quantifiable nature of the data, which can be archived for objective comparisons. For example, some orthoses may be prescribed to control excessive ankle equinus and prevent knee recurvatum during gait. The only way to be sure an ankle-foot orthosis is achieving this effect is to compare data with and without it.
Even more important, some surgical interventions that may improve ambulation require a year or more of rehabilitation to recover to presurgical status. One of the most objective measures of surgical outcomes can be obtained through gait analysis in which preoperative data is compared to postoperative data. Joint angles and moment curves that move toward “normal” would be evidence of a positive surgical outcome, augmenting clinical findings of functional improvements in walking speed, balance, and endurance.
FINANCIAL CHALLENGES
For all the benefits of using CGA in rehabilitation, the cost of doing so may be a drawback. The initial capital outlay required to obtain the necessary hardware, software, and personnel to interpret the data is significant. Consequently, there are fewer than 100 dedicated clinical gait analysis facilities in the nation.
Billing often presents a challenge as well. Many third-party payors regard CGA as experimental, forcing many institutions to operate CGA facilities at a loss until payors recognize their value. For patients, the value may be immeasurable if it means an optimal combination of procedures at an optimal point in time, requiring only one bout of postintervention rehabilitation. Thus, bringing technology into the rehabilitation process early may help clinicians optimize a treatment plan sooner rather than later, benefiting patients and payors alike.
Moving forward, CGA labs are pushing to improve biomechanical models and document the impact of the analysis on subsequent care. Clinicians and patients involved with gait rehabilitation can benefit greatly from technology that enhances treatment decisions and improves the ability to measure outcomes.
Krisanne B. Chapin, PhD, is the manager and clinical biomechanist of the Motion Analysis Center at Mary Free Bed Rehabilitation Hospital, Grand Rapids, Mich. Chapin, who holds degrees in biomechanics and exercise and movement science, has been practicing gait analysis for 10 years. For more information, contact .




