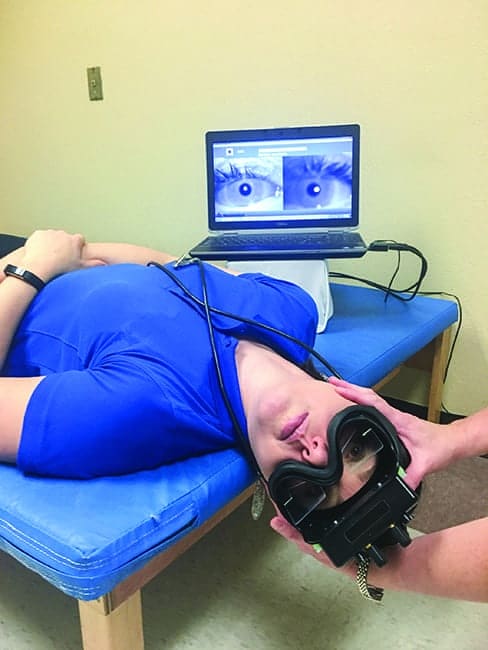
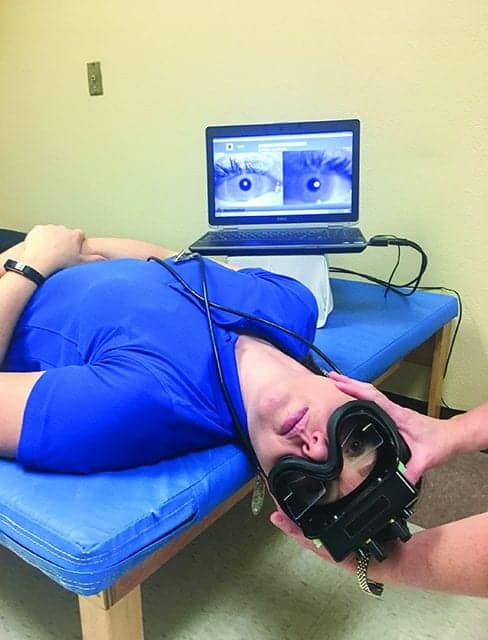
Video goggles during a Hallpike maneuver used to magnify and record the eyes during an assessment for left posterior canal BPPV. (Optional fixation block not featured to allow visibility of testing position.)
by Susan Kreinbrook, PT, MPT
Patients in need of vestibular rehabilitation present a myriad of symptoms and can be helped by a wide array of healthcare practitioners, including family physicians, otorhinolaryngologists, neurologists, physical therapists, occupational therapists, speech language pathologists, psychologists, psychiatrists, audiologists, and VENT technicians.
Physical therapists play a critical role in the rehabilitation of individuals suffering from vestibular disorders throughout the continuum of care. They also act as an important voice in the multidisciplinary approach that makes up an effective treatment team for these patients. Therapy for vestibular disorders takes on many forms and is as unique as the symptoms that each client demonstrates or reports. Technology is an important tool that can be utilized to effectively evaluate and treat such a diverse patient population. Following are some of the more effective and common technologies that specialize in treating the vestibular patient.
Video Goggles
Video goggles are worn over the eyes, similar to swim goggles, and can provide a definite advantage to the evaluation process. Many video goggles have the capacity to magnify the eye, display it on a screen, and record the session. Options, such as room cameras and goggles that can record one or both eyes, can add to the ease and accuracy of data collection and can be helpful for staff training, research, or teaching purposes.
At HealthSouth Harmarville Rehabilitation Hospital, Pittsburgh, a hospital in the Encompass Health Corporation network, binocular video goggles are utilized on both outpatients and inpatients. In my capacity as a physical therapist there, I have seen patients in inpatient rehabilitation admitted with dizziness from acute care where they were unable to be stabilized or resolved. We use our video goggles to diagnose them and successfully resolve their symptoms, oftentimes in just one session. This allows the inpatient team to then focus on restoring their mobility, and they return home with a higher level of independence and reduced disability. One patient I evaluated with the video goggles at the hospital reported, “I have been falling down the stairs for 3 months because every time I looked down I felt dizzy. Now I have the confidence to move around my house without being scared.” As opposed to compensating for the dizziness with medication, which simply reduces symptoms, the video goggles allowed me to treat her for benign paroxysmal positional vertigo (BPPV) and initiate a treatment plan that focused on mobility and restoration of function.
A fellow therapist from the rehabilitation team reported that the benefits of using video goggles allowed her to minimize repeat testing on a patient because she can often see the issue more clearly during the initial testing. She has the option to watch the recorded video again without putting the patient through the symptom-producing test a second time. Success with initial testing is crucial when working with an individual who becomes nauseous, anxious, and/or experiences pain from comorbidities with the testing.
“Keeping the patient calm and comfortable are definite advantages of the equipment that we use at this facility, such as video goggles,” says Kristy Herlihy, PT, DPT, at HealthSouth Harmarville.
Many of the goggles weigh less than 1 pound and feature a cap to prevent a patient from fixating their gaze. Fixation can reduce or eliminate their nystagmus. Magnification of the eyes is also beneficial when attempting to interpret the directionality and/or presence of nystagmus, phoria, or tropia. A very common use of the goggles is examination of the suspect BPPV client. Specific maneuvers are decided upon by this information, and 85% of patients recover from BPPV when treated with these maneuvers by a physical therapist or physician.
Convergence insufficiency, a common issue in the post-concussive patient, as well as many central vestibular abnormalities, can also be identified by use of the goggles. Personally, video goggles help me to identify the overshooting/undershooting associated with central vestibular dysfunction with saccade testing, corrective saccades with smooth pursuit testing, and any resting nystagmus that may occur when not allowed to fixate.
Proper examination and creation of a problem list will allow the most effective treatment and symptom resolution to optimize outcomes for the vestibular patient. I once treated a client who lived about an hour away and had been seen at a hospital without this technology for a concussion that occurred from hitting her head after falling on ice. Upon examination, I discovered she had BPPV and, upon treatment, her symptoms completely resolved after one maneuver. I discovered she had been tested in the same manner for BPPV at another hospital, but without the use of the goggles, and her results for BPPV were negative. Due to this, she was never treated, and her symptoms were assumed to be concussive, not BPPV-related.

Computerized balance system to assess sensory organization, limits of stability, and fall risk. This technology can allow the therapist to target interventions that maximize outcomes and also allow the ability to track outcomes.
Computerized Balance Systems
Computerized balance systems are also a helpful tool in examining the balance system and teasing out the impairments and their source. Balance comes from our three main systems: vision, vestibular, and proprioception. Many of the computerized balance systems have the capacity to run tests and reports that analyze which systems are in deficit and need training. Fall risk management and balance optimization have the potential to prevent further injury, promote more confident and independent mobility patterns, and reduce the disability that is created by an insufficient balance system. Many of the computerized systems have normative data, which allows the clinician not only to see how the patient does but also immediately compare it with their age-related peers. This can be helpful for patient education, exercise prescription, and reimbursement challenges. I have found that sending reports to physicians and insurance companies, as well as showing them to patients and family members, enhances the interdisciplinary approach, and provides access to and coverage of physical therapy services and compliance with home exercise programs, respectively. When patients understand their limitations, they are more likely to put in the work to correct them.
Patients who utilize the outpatient services at HealthSouth Harmarville not only benefit from review of testing performed on the computerized balance machine, but also training on it, as it has an interface screen that provides immediate feedback on center of mass, limits of stability, and weight-shifting/weight-bearing abilities and deficits. One client with post-concussion syndrome stated, “This allowed me to see what I need to do, and it also makes my eyes tired.” He goes on to comment after a few weeks of training at three times each week for 15 minutes during his sessions that, “I can read now without the page blurring after 2 minutes, and I know that the computerized balance system is why.”
Utilizing the unstable surface feature for testing and treatment can enhance reaction speeds for the patient with fall risk and difficulty on uneven terrain. Drills and training on such equipment often can create motor skills that carry over to situations that put the client at risk of falls and injury.
Rotational Chair Tests
Not all technology that can benefit a patient’s exercise prescription is performed in the physical therapy gym. Oftentimes rotational chair tests allow the clinician to ascertain what is occurring with the vestibular system, and when the prescription for therapy comes over with reports including this technology, the skilled therapist can properly tailor not only their exam but also future treatments and recommendations to optimize outcomes. The advantage of a rotational chair test is that many of them provide a dark room enclosure with eyes-uncovered recording. They utilize multidirectional laser projection for oculomotor testing often projecting static and/or moving items on the wall. This is very difficult to establish without this technology. Response to rotation and the resultant nystagmus can evaluate whether the dizziness is due to the inner ear or the brain and is an excellent way to diagnose bilateral vestibular loss. This will allow a report to be generated and a more focused exercise prescription to be developed that drives improved outcomes for these patients. Many patients with dizziness or traumatic brain injury (TBI), and athletes with chronic traumatic encephalopathy can benefit from such examination.
Technology’s role in the examination and treatment of the vestibular patient cannot be understated. This article offers just a small example of how therapists, physicians, and audiologists are utilizing technology to diagnose, educate, and treat such clients. Research on each of these devices also helps us prescribe and dose interventions and justify our role to drive reimbursement and access to services.
Clinics that utilize these technologies and/or possess the experience to interpret the results of reports from these technologies may be considered to have an edge in treating the vestibular client. Whatever the case, vestibular therapy is most often a multidisciplinary approach that utilizes the skills of many players in the healthcare system. Technology can allow us to see which role may be the most important and how to streamline treatment and improve the accuracy of our exam and effectiveness of our interventions as therapists, physicians, and technicians. RM
Susan Kreinbrook, PT, MPT, has been a practicing physical therapist since graduation from Duquesne University in 2003. She has been involved with treating vestibular clients since 2005, and is a senior therapist involved with the vestibular program providing outpatient and inpatient consults to those with various vestibular disorders. Kreinbrook works with a wide variety of vestibular issues including BPPV (benign paroxysmal positional vertigo), central vestibular disorders, Meniere’s disease, concussion, as well as the symptoms of vertigo, imbalance, and dizziness. She utilizes the multidisciplinary approach of vestibular treatment working with neurologists, audiologists, ENTs, speech language pathologists, and psychiatry to treat all aspects of the vestibular patient. For more information, contact [email protected].





I had no idea that therapy for vestibular disorders takes on many forms and is as unique as the symptoms that each client demonstrates. My son recently got diagnosed with a vestibular disorder, and might soon be starting vestibular therapy. I will keep all of your information on vestibular therapy in mind if my son does start therapy.