 |
On November 15, 2006, CMS implemented new power mobility devices (PMD or power wheelchairs) codes and policies. There are now 64 codes with six groups: Group 1, light use; Group 2, consumer rehabilitation; Group 3, complex rehabilitation; Group 4, high-activity use; Group 5, pediatric; and Group 6, miscellaneous, including power push rims and add-on power packs.
|
Group |
Description |
|
1 |
Light-Use |
|
2 |
Consumer Rehab |
|
3 |
Complex Rehab |
|
4 |
High-Activity Use |
|
5 |
Pediatric |
|
6 |
Miscellaneous (incl power push rims and add on power packs for manual wheelchairs) |
Each group is further divided by type of seat (sling, solid, and captain), power options (no options, single, and multiple), and weight capacity (standard and heavy, 301 to 450 pounds; very heavy, 451 to 660 pounds; and extra heavy, more than 601 pounds). A single power option is needed for one feature (for example, “tilt”). If the client needs tilt and recline (or any two or more features), they would require the multiple power option.
Every PMD must include (in the basic price) footrests (including angle adjustable), positioning/safety belt, seat, back, non-height-adjustable armrests, battery, and charger. The supplier cannot charge for these items individually. Every PMD must be submitted to CMS for coding and be crash tested. If the device has not been approved by CMS, it will not be covered by Medicare.
STRICTLY DEFINED CRITERIA
The criteria for qualification for a PMD have been strictly defined. The client must have a mobility limitation that impairs their ability to participate in one or more mobility-related activities of daily living (MRADLs), including toileting, feeding, dressing, grooming, and bathing in the home. This limitation can prevent the client from accomplishing the MRADL entirely, or from completing the MRADL within a reasonable time frame. This means that if a person needs a PMD to complete their morning MRADLs quickly—so they can, for example, get to work or school—they may be able to get that PMD. In the past, a recommendation may have been included in the letter of medical necessity (LMN), a reference for the need to use the PMD to get to and from work, or for a client to perform their daily job tasks. Now we take all that out and describe only how a PMD enables a person to get ready in the morning, at home, in a “reasonable amount of time.” A person also might be eligible for a PMD if, without this device, they are at a heightened risk of morbidity or mortality, secondary to the attempts to perform an MRADL without the PMD. It is essential that the LMN use the proper language and descriptions. Some states, such as Washington, have forms available that make the process more quick and efficient. (CMS cautions that the form still needs to include all the pertinent information.)
CHANGES FOR THERAPISTS
 |
| When providing information for a client’s letter of medical necessity for a PMD, the therapist must address several points on a CMS checklist. |
One change for physical therapists and occupational therapists is that the evaluating and recommending therapist cannot be tied financially in any way to the supplier. The only exception is when the health care system owns the therapy practice (hospital, outpatient physical therapy clinic, etc) and the supplier.
The biggest change will come in April 2008 when all physical therapists and occupational therapists will be required to have ATP certification to assess and recommend all equipment and assistive technology funded by Medicare. Will other third-party payors follow? This is a huge issue. For clients, access may be limited since there are so few non-supplier-linked ATP credentialed therapists, especially in rural areas. Will physical therapists and occupational therapists need to be credentialed by engineers? Should AOTA and APTA be responsible for this process? Or is the ability to complete a PMD assessment already mandated through our practice acts? This will be an ongoing debate, and it may not be resolved by April 1, 2008, when the new regulations go into effect. If physical therapists and occupational therapists want to continue to be able to do PMD assessments, they will need to either sit for the RESNA examination, and/or work with the AOTA/APTA to figure out a solution.
MORE CHANGES
Single power options will be covered only for clients who require a drive control other than a hand or chin control and/or the client meets the criteria for tilt or recline. To justify tilt and/or recline, the LMN must state and support that the client meets one of the following three criteria: is at high risk for pressure sores and cannot perform an adequate weight shift, client requires intermittent catheterization and cannot independently transfer from PMD to bed, and/or the power seating system is required to manage increased tone or spasticity.
To qualify for funding for the multiple power option, the LMN must support and state that the client qualifies for tilt and recline and/or uses a ventilator that is mounted on the PMD.
For Group 5 (pediatrics), the LMN must document that the child cannot transfer independently due to a neurological condition or myopathy.
Power push rims are covered only when the client has been self-propelling for 1 year and meets the criteria for Group 1. Add-on kits that convert a manual wheelchair to a PMD will not be covered.
|
Group |
Codes |
Required Components |
|
1 |
K0800 |
PMV/Scooters PMD, portable, sling/solid seat/back, up to 300lb client |
|
2 |
K0820 |
PMD, portable, sling/solid seat/back, up to 300lb client |
|
2 |
K0835 |
Single power option, sling/solid seat/back, up to 300lb client |
|
2 |
K0841 |
Multi power option, sling/solid seat/back, up to 300lb client |
|
3 |
K0848 |
Standard, sling/solid seat/back, up to 300lb client |
|
3 |
K0856 |
Single Power Option, sling/solid seat/back, up to 300lb client |
|
3 |
K0861 |
Multi Power Option, sling/solid seat/back, up to 300lb client |
|
4 |
K0868 |
These are all PMDs that have capabilities that are not needed for use in the home.Payment will be based on the Group 2 or 3 PMD that meets the client’s medical needs, but they may pay out of pocket for the upgrades. |
|
5 |
K0890 K0891 |
Pediatric, single power option, sling/solid seat/baclk, up to 125lb client |
|
6 |
K0898 E0983 E0984 E0986 |
POWER WHEELCHAIR, NOT OTHERWISE CLASSIFIED |
For more information on Region A/B PSC Local Coverage Determination (LCD) for power mobility devices, go to www.tricenturion.com, and type “power mobility devices” in the search engine.
LETTER OF MEDICAL NECESSITY/JUSTIFICATION
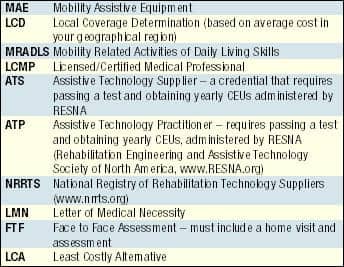 |
The LMN must be written by the licensed/certified medical professional (LCMP)—the physician, physical therapist, or occupational therapist who did the face-to-face assessment. The date is very important, as there are now strict timelines to follow (45 days from evaluation to the time the report must be received by supplier). Delivery must occur within 120 days following the face-to-face assessment. The LCMP can have no financial ties to the supplier (and cannot be compensated for their time in any way), except in the case where the health system owns the medical center or clinic and the supplier. After April 1, 2008, the person recommending the equipment (physical therapist or occupational therapist) will need to be a RESNA-certified ATP. The LCMP must clearly indicate that a major reason for the visit was a mobility examination.
THE PHYSICIAN’S ORDER
The order that the supplier must receive within 45 days after completion of the face-to-face examination must contain all of the following elements: 1) The beneficiary’s name; 2) A description of the item that is ordered. This may be general, for example, “power-operated vehicle” (POV) or “power mobility device,” or it may be more specific; 3) Date of completion of the face-to-face examination; 4) Pertinent diagnoses/conditions that relate to the need for the POV or power wheelchair; 5) Length of need; 6) Physician’s signature, and 7) Date of physician signature.
WRITING THE LMN
When providing information for the client’s letter of medical necessity, some of the points that need to be addressed are:
- What is the client’s mobility limitation and how does it impact ADLs?
- Why a cane/walker/manual wheelchair/scooter cannot meet the client’s needs pertains only to in the home (leave out any references to community);
- Does the client have the physical/mental abilities to operate the PMD safely in the home? Will the home accommodate the PMD (for example, door widths and turning radius)? Does the client want the PMD?
- Symptoms, related diagnoses, history, and predicted clinical course/progression/degeneration;
- Interventions (equipment) that have been tried, and the results;
- Physical examination and weight;
- Actual measurement (must use reproducible measurements) of strength, ROM, sensation, motor control, tone, spasticity, etc;
- Sitting/standing balance and transfer ability;
- Can the client walk between rooms in their home; and
- The length of need.
Additional Points on the Checklist:
- Symptoms
- Related diagnoses
- History
- How long the condition has been present
- Clinical progression
- Interventions that have been tried and the results
- Past use of walker, manual wheelchair, POV, or power wheelchair and the results
- Physical examination
- Weight
- Impairment of strength, range of motion, sensation, or coordination of arms and legs
- Presence of abnormal tone or deformity of arms, legs, or trunk
- Neck, trunk, and pelvic posture and flexibility
- Sitting and standing balance
- Functional assessment—any problems with performing the following activities including the need to use a cane, walker, or the assistance of another person
- Transferring between a bed, chair, and PMD
- Walking around their home—to bathroom, kitchen, living room, etc—provide information on distance walked, speed, and balance
- A date stamp or equivalent must be used to document receipt date. The written report of this examination must be available on request.
WHAT SHOULD YOU DO?
 |
| New CMS coding makes it more complicated for users to qualify for power mobility devices. |
For rehabilitation professionals, my best advice is to call or contact your favorite PMD manufacturer and sign up for one of their Web courses on the new codes. A number of companies are offering a variety of seminars, and there will be special sessions at the 2007 International Seating Symposium in Orlando, Fla. If you are a physical therapist or occupational therapist and routinely assess for PMDs, it is probably time to sign up for a study group and apply to sit for the examination for the ATP credential. Also, getting active with AOTA or APTA to help figure out how to credential ourselves is another great idea. If you are a supplier, it is time to join the National Registry of Rehabilitation Technology Suppliers (NRRTS)—and their fabulous Listserve. This is just the beginning. While these changes affect only Medicare today, other third-party payors may follow. CMS will now move on to changes in manual wheelchairs and then go through the remaining categories. Doran Edwards, MD, medical director of the Statistical Analysis Durable Medical Equipment Regional Carrier (or SADMERC), and CMS are very responsive to public opinion. The more letters and ideas they receive from end users, therapists, physicians, and suppliers, the better informed they will be. The NRRTS and industry leaders, like Rita Hostek, have done an amazing job (and spent thousands of dollars and hours) to aid CMS and SADMERC in their coding decisions. We should continue to work together to decrease fraud and help our clients get what they need.
Power mobility insiders are acutely aware of the need to stay informed of the fluctuating changes affecting the marketplace, and are positioning to remain a united force. According to Marilyn Hamilton, director of education at a major power mobility manufacturer, “Our world is changing. As the dust settles, it is more important than ever that the industry understands the most up-to-date information regarding the recent changes in PMD coding and funding changes. That is why [our company] is hosting a series of Web-based seminars designed to navigate changes addressing issues and concerns of the clinical community.”
 |
| In the criteria for qualifications for a PMD, a therapist must include assessment of impairment of mobility and range-of-motion limitations. |
Tara Gentile, funding project specialist for a Lebanon, Tenn-based developer of innovative power wheelchairs, comments, “The new codes, policies, and reimbursement schedule will continue to affect our business as well as the entire industry. Under the old and new rules, [our company] is faced with the same challenge—ensuring the consumers receive the most appropriate equipment, regardless of funding.
“Our customer base is made up of only certified providers [for our products], truly the best rehab providers in the country. Our salespeople are trained, certified professionals. We are committed to partnering with our certified providers, so that they can continue to offer the same level of services our consumers deserve. Our mission is to enhance lives. People are depending on us. We’ll make it work,” adds Gentile.
Kevin Quaglia, general manager of industry relations of a leading manufacturer of electric scooters, lift chairs, and power wheelchairs, says, “[Our company] is committed to providing education for clinicians and providers about the changes in coding and coverage for PMDs. Through our annual seminar series, Internet-based Webinars, and online documents (on our provider and clinician Web site), we will continue to educate all industry stakeholders on these important changes.”
For updates regarding these changes, go to www.trustsolutionsllc.com/MedPolicies/PMD%20R2%20Final%20Draft.htm.
Ginny Paleg, MS PT, a pediatric physical therapist with the Montgomery County Infants and Toddlers Program in Rockville, Md, is a reimbursement representative for the pediatric section of the APTA, and teaches continuing education courses for several DME manufacturers. Paleg also is a member of Rehab Management’s editorial advisory board. She can be reached at .





