
As a physical therapist who has treated athletes for more than 20 years, I have come to realize there is a distinct and unique way I treat athletes. They present unique challenges that make assessment and treatment different from any other group of patients, which in turn requires a unique skill set necessary for complete recovery and return to sport. When an athletic physical therapist understands the underlying philosophy and can implement a solid treatment methodology, new levels of success can be achieved.
ATHLETIC PHYSICAL THERAPIST PHILOSOPHY
Know the Body
Skilled physical therapists have a three-dimensional picture painted in their minds about what lies beneath the surface of the skin. It takes years of training and study to be able to think on your feet and imagine how bones, nerves, cartilage, muscles, vessels, and ligaments glide, slide, contract, and relax. There is a logical evaluation progression that must be followed; however, there must also be a keen intuitive sense. It is the obligation of the physical therapist to know the exact relationship between all of the various tissues and structures in the human body so that the physical therapy diagnosis focuses on physical impairments as they relate to functional limitations that prevent the athlete from returning to a preferred sport.
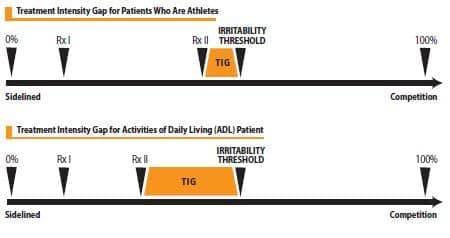
Figure 1. Treatment Intensity Gap (TIG)
Know What You’re Treating
Going through a “classroom evaluation” is neither effective nor efficient in a busy private practice physical therapy setting. A master physical therapist will have 50% of the physical therapy diagnosis determined after understanding the subjective findings. It is during the history of the evaluation that the athletic physical therapist systematically collates and organizes all of the assessment tools down to only those necessary. Once the objective assessment begins, the therapist should already know the logical progression of assessment tools needed to complete an accurate physical therapy diagnosis. It is only when the physical therapist combines the medical diagnosis, physical therapy diagnosis, objective assessment, and patient goals that they will truly understand the restorative requirements necessary for the injured tissue to survive game time challenges.
Maximize Your Treatments
The athlete’s injury should be placed on an imaginary time line somewhere between full athletic competition and being sidelined at a point called the irritability threshold. The threshold is a variable point in time during the active rehabilitation continuum when a subjective reproduction of symptoms occurs and/or an objective assessment of impairments is measured indicating that the injured tissue is unable to meet the current level of demands necessary for the requested athletic activity. When the threshold is low, small amounts of stress through the injured tissue can provoke an undesirable response to treatment. Conversely, when the irritability threshold is high, the tissue is not easily provoked.
The athletic physical therapist’s first treatment objective is to avoid provoking the injured tissue and exacerbating the condition. I purposefully initiate treatment (Rx I) so that I am certain to not make the patient worse after the first visit. This may sound strange, but it is far easier to speed up a treatment than to go backwards and have to slow down. I tell athletes that the first treatment may seem submaximal, but I want them to come back and tell me that they don’t feel worse. After I’ve initiated treatment and established the baseline of nonprovocation, I can confidently accelerate my treatment (Rx II) intensity to just below the irritability threshold without exacerbating the injury or condition. It is being aggressive but not careless that allows me to deliver the exact dose of treatment necessary to maximize the recovery process. This, in turn, accelerates return to sport.
The difference between RxII and irritability threshold is called the Treatment Intensity Gap (TIG) (Figure 1). Athletic physical therapists should make this gap as small as possible so that each treatment is just below the irritability threshold. This also means treatment itself is most likely painful, but after the treatment, symptoms are not increased. Physical therapists who are trying to restore ADL can maintain a wider TIG, which will make the treatment more comfortable for the patient.
Competition
Now that we have the philosophy behind what it takes to be an effective athletic physical therapist, let us look into a case example using a treatment model called the Active Rehabilitation Continuum or ARC.

Figure 2. Stage III end range open chain knee flexion with combined tibial external rotation.
CASE REPORT
A high school football player sustained a knee injury while playing quarterback in a spring passing league. He was preparing for his junior year, and at 6’2,” 220 pounds, he was already a serious NCAA Division I prospect. Following a MRI, he was diagnosed with a Grade II MCL strain, which was confirmed through the physical therapy assessment. He presented 1 week following his injury using two axillary crutches and a non-weight-bearing gait, hoping to return to a invitational football camp in 6 weeks. This patient presented numerous challenges that could make successful rehabilitation difficult for even the most skilled. Utilizing the Athletic Physical Therapist Treatment Philosophy and the Active Rehabilitation Continuum, I created a physiological tissue healing environment and a comprehensive framework to maximize treatment results.
The ARC and irritability threshold treatment methodology were first introduced in 2005. The ARC consists of three stages called “The Power of Three,” which provides purposeful guidelines to assist the therapist in understanding treatment bias for manual therapy, phases of functional exercise progression, the inflammatory threshold, and return to sport participation progression.
ARC METHODOLOGY: THE POWER OF THREE
Stage I
Stage I of the ARC includes the first 2 weeks post-injury and is considered the inflammation phase of healing. During the first week, rest, limited weight-bearing, protection of the injured tissue, and immobilization are often prescribed. In the second week, physical therapy may begin including manual therapy consisting of gentle and progressive passive and active/active assistive range of motion, paying special attention to avoid excessive stress through the healing tissue. Generally, no strengthening is done in this phase; however, activities such as walking, light active range of motion, and nonresistive proprioceptive neuromuscular facilitation can be initiated. There is obviously no sport participation, and the patient’s irritability threshold is low, meaning that it doesn’t take a lot to elicit a negative response to therapy or activities. Anti-inflammatory modalities such as electrical stimulation, laser, and ice are incorporated.
- Inflammatory threshold: Low, highly irritable.
- Treatment bias: anti-inflammatory or tissue healing treatments with mostly manual skills/modalities to create a healing environment for injured tissues.
- Therapeutic exercises: Phase 1 is low load, controlled speed, and limited duration and frequency, and is performed in a supported, controlled, and isolated manner.
- Sports participation: observation only.
Stage II
Stage II of the ARC generally lasts between 2 and 4 weeks and is considered the proliferation phase of healing. The proliferative phase of the healing process includes cell differentiation and revascularization. Stretching becomes important so that the structural and functional alignment of the collagen fibers can be achieved. Manual therapy consists of progressive grade II-IV joint mobilizations and stretching so that full range of motion is restored. The exercises include phase 2 lightly loaded and limited range of motion, functional exercises progressing toward phase 3 complex, multiplanar and loaded exercises. Activity participation is progressed from none to limited and then to modified. The inflammatory threshold is improving toward medium and then high as the patient becomes less irritable and gains strength.
- Inflammatory threshold: Medium to high, moderately irritable.
- Treatment bias: continuation of manual therapy techniques, decrease in use of modalities progressing to moderate intensity manual therapy for tissue remodeling and neuromuscular reeducation.
- Therapeutic exercises: Phase 2 and 3 are multijointed, complex movement patterns with a medium load, speed, duration, and intensity.
- Sports participation: Modified participation to begin Athletic PT Sport Specific interval program with MD consent.
In this particular case, during stage II of the ARC, sequential treatments included the use of manual therapy tools. These tools are part of a growing concept within rehabilitation that incorporates instrument assisted soft tissue massage (IASTM) techniques to facilitate and enhance the healing process. The tools were used during the remodeling phase to align collagen fibers in the healing phase directly on the MCL.
Stage III
Stage III of the ARC includes the remodeling phase of the natural healing process and can last between 5 and 12 weeks. Manual therapy consists of complete, end range of motion and activity-specific joint mobilizations necessary to return to competition or preferred sport activity. The phase 4 functional exercises consist of fully loaded and full range of motion activities progressing into phase 5 high-speed, plyometric, power, and sport/position specific exercises. The irritability threshold is high to nonexistent, and the patient does not have flare-ups following participation or activity.
- Inflammatory threshold: None, nonirritable.
- Treatment bias: discontinuation of modalities and aggressive manual therapy techniques involving torque through a joint with grade IV mobilizations.
- Therapeutic exercises: Phase 4 and 5 fully loaded, athletic functional exercises are performed with increased speed designed to simulate sport-specific conditions and prepare for athletic competition and completion of Athletic PT Sports Interval Program.
Sports participation: full return.
The manual therapy and stretching performed on the lower extremity are for the competitive athlete only as they place significant stress and torque through the knee to simulate the forces necessary to return to sport.
Understanding the philosophy and methodology of athletic physical therapy is important so that expedited and positive outcomes are realized. It is also mutually beneficial to the therapist and athlete to set meaningful and distinctive benchmarks from which the therapist can advance the patient. This allows the patient to recover in the shortest period of time while avoiding unwanted setbacks. RM
Stephen Clark, PT, DPT, OCS, MBA, is the president and founder of Athletic Physical Therapy Inc, a sports and orthopedic private practice with multiple locations in Los Angeles and Ventura counties, California. For more information contact .





