 |
Before the departure of former Centers for Medicare and Medicaid Services (CMS) Administrator Mark McClellan, MD, PhD, last October, a critical reform plan was unveiled related to this country’s post-acute care (PAC) health delivery system.
Over the past few years, CMS has urged senior leadership to develop strategic policy directions and initiatives to improve the nation’s health care system. CMS believes that the post-acute care product is not well defined. Differences in assessment instruments make detailed comparisons across the settings difficult and/or impossible. Without a uniform patient assessment methodology for post-acute care patients, CMS believes the result is care fragmentation, unsafe care transitions, and inability to determine cost-effective settings for each patient discharged to post-acute care. Therefore, one of the most important priorities was to develop a plan for post-acute care reform.
The CMS post-acute care reform plan addresses three main areas: (1) the current problems in the PAC system; (2) CMS’ principles and vision for post-acute care reform; and (3) various short-term and medium-term steps toward that goal.
POST-ACUTE CARE PAYMENT SYSTEM DIFFICULTIES
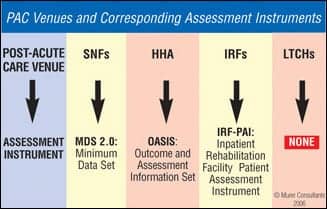
Medicare currently provides reimbursement for post-acute care services in the following inpatient settings: skilled nursing facilities (SNFs), home health agencies (HHAs), long-term care hospitals (LTCHs), and inpatient rehabilitation facilities (IRFs). For each of these post-acute care provider settings, there is a separate prospective payment system.
Three of these payment systems (SNF, HHA, and IRF) rely on standardized data collected by providers using assessment tools developed for multiple purposes, including assessment, quality improvement, and payment. Currently, no assessment instrument is mandated for long-term care hospitals. Since there is no uniform assessment instrument throughout the entire post-acute care health care delivery system, all data is collected in different formats, which are often incompatible. This incompatibility makes it difficult to compare beneficiaries and their use of services and items across post-acute care settings. (See Chart #1 below.)
 |
| Chart #1 |
Additionally, Medicare’s PAC benefits and payment policies focus on phases of a patient’s illness defined by a specific service site, rather than on the characteristics or care needs of the Medicare beneficiary. Accordingly, payments across the various post-acute care settings can differ considerably even though the clinical characteristics of the patient and the delivered services may be very similar.
CMS PRINCIPLES AND VISION
The primary focus of CMS’ vision for post-acute care is for the system to become patient-centered. In other words, the system will be organized around an individual beneficiary’s needs rather than around the settings where care is delivered. This vision defines post-acute care in terms of patient populations needing care. Specifically, post-acute care is care that is provided to individuals who need further support to assist in recuperation following an acute illness or serious medical procedure.
CMS believes that a more beneficiary-centered system of the post-acute care sector will help improve the quality and continuity of care in a cost-efficient manner. CMS has stated that the person-centered post-acute care system of the future will:
- Optimize choice and control of services;
- Ensure that placement decisions are based on patient needs with both the patient and their family receiving honest and useful information about the patient’s situation and prognosis;
- Provide coordinated, high-quality care with seamless transitions between settings;
- Reward excellence by reflecting performance on quality measures in payment;
- Recognize the critical role of family caregiving; and
- Use health information technology.
Ultimately, CMS desires to increase consumer choice and control of post-acute services. CMS also believes that a seamless continuum of care for beneficiaries is necessary and that improved coordination of acute care, post-acute care, and long-term services is required to achieve this goal. CMS has a goal for post-acute care providers to provide high-quality PAC services in the most appropriate setting based on patient needs. This will require moving patients through the continuum of care into the right PAC venue at the right time.
Another principle of the CMS post-acute care reform plan involves developing effective measures in order to drive the PAC system toward the delivery of high-quality care in the most effective manner, which will ultimately improve payment efficiency.
THE PATH TOWARD ACHIEVING REFORM
To improve the accuracy of quality measurements and the comparability of results across post-acute care facility types and to improve the accuracy of payment for post-acute care, CMS is developing a Post Acute Care Payment Reform Demonstration based on a Congressional mandate (Deficit Reduction Act Section 5008). CMS’ analysis suggests that the separate payment systems, patient assessment forms, and requirements lead to problems with care continuity, the inability to compare quality results across settings, and inappropriate incentives for transfer and care provision. CMS will take action to address these concerns by:
- Developing a patient assessment tool to be used in acute care hospitals and in PAC settings, including LTCHs, IRFs, SNFs, and HHAs;
- Developing a cost collection tool to access resource use in the four PAC settings; and
- Designing a large-scale implementation of the new patient assessment tool and cost collection tool with the intent to reform payment across the four sites based on the information collected.
This demonstration is mandated for a 3-year period and is to include a sufficient number of sites to ensure statistically reliable results. Within 6 months after the demonstration, the CMS Administrator must report to Congress on the results and make appropriate recommendations.
The uniform assessment instrument being developed under the demonstration will be comprehensive, interoperable, and implemented on an Internet-based platform. In addition to use within the demonstration, the uniform assessment instrument will be made available for use by outside hospitals of the demonstration in 2008 on a voluntary basis as a tool for improving care transitions to post-acute care settings. CMS’ goal is that the assessment and cost data collected under this demonstration will lead to a comprehensive, site-neutral post-acute care payment reform.
In addition to the PAC payment reform demonstration, CMS also outlined pay-for-performance plans in the post-acute care sector. CMS currently has activities under way regarding pay-for-performance for both the home health and the skilled nursing facility settings. Starting in 2007, CMS began pay-for-reporting. HHAs that submit the required quality data will receive payments based on the full proposed home health market basket update of 3.1% for CY 2007. If the HHA does not submit the quality data, the market basket percentage increase will be reduced by 2% points to 1.1% for CY 2007. Pay-for-reporting will eventually transition to pay-for-performance.
In regard to skilled nursing facilities, CMS anticipates implementing a 3-year Nursing Home Value Based Purchasing Demonstration under which participating nursing homes will be offered financial incentives to provide high-quality care and to improve the level of care they provide.
Additionally, the FY 2007 President’s Budget includes a proposal to reduce the excessive difference in payment between inpatient rehabilitation facilities and skilled nursing facilities for the treatment of total knee and hip replacement beneficiaries. CMS also is committed to finding opportunities to propose policies that further the program in the direction of the ultimate goal of site-neutral payment for post-acute care services.
CONCLUSION
Ultimately, CMS is attempting to ensure that post-acute care placement decisions are made on a patient-centered basis rather than economic incentives. The current differences in the post-acute care payment systems have created a system that makes precise comparisons across the post-acute sector impossible.
The development of a uniform patient assessment tool will help ensure the smooth flow of patient information from the acute to the post-acute setting. It also will help guarantee that the patient’s medical need is the primary concern in movement of the patient through the continuum of care. The current research being done in accordance with CMS’s post-acute care reform plan parallels that which took place on prospective payment in the 5 to 10 years before the implementation of the post-acute care prospective payment systems.
Thus, while the implications of the post-acute care reform plan may have little immediate impact, there is every reason to believe that we are in the first stages of research that will determine the role post-acute care venues will play in Medicare in the next 5 to 10 years.
Cherilyn G. Murer, JD, CRA, is CEO and founder of the Murer Group, a legal-based health care management consulting firm in Joliet, Ill, specializing in strategic analysis and business development. Murer may be reached at (815) 727-3355, or viewed on her Web site at www.murer.com.




