A focus on developing coordinated muscle strength protects the patient-athlete’s spine from injury.
Whether patients are professional athletes, recreational athletes, or injured workers, they often share the same goal after spine surgery: to return to the highest level of function with the least amount of pain. And nearly all patient-athletes express their greatest concern after spine surgery with a question, “When can I return to play?” The answer depends primarily on two factors. The first is an effective minimally invasive surgery. The second is a proper postoperative rehabilitation program. Those elements must be united under a coordinated effort between physician, patient, physical therapist, and the patient’s employer, for athletes to make their quickest return to sports. To that end, our practice has developed a structured core stabilization program that allows all stakeholders in the recovery process to easily monitor and guide recovery.
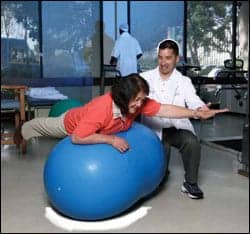
After successful spine surgery, our program moves the patient-athlete’s recovery process forward through a five-level program that gradually increases demands on strength, endurance, and proprioception. The patient-athlete progresses through eight different exercises—rated one through five in difficulty—that produce functional coordinated core strength for the body. These exercises aim to develop coordinated muscle strength to achieve maximum performance while protecting the spine. The importance of this process is underscored in testing of professional golfers, major league baseball players, and other athletes, which points to the coordination of trunk muscles as a way to produce maximum control of the spine.1 These tests demonstrate that coordinated strength is more effective than uncoordinated strength because each of the trunk muscles fires in an exact sequence in relation to the other in the performance of a particular action. This program develops coordinated strength to protect the patient-athlete’s spine from injury as well as to produce the desired athletic result.
SIMPLICITY AND STEPS TO SUCCESS
The program begins with the patient finding a neutral, pain-free position for the spine and strictly holding the spine in that position while performing exercises. This makes it possible to begin postoperative conditioning earlier by avoiding extremes of motion through the injured spine. The entire program can be performed with relatively simple equipment: exercise balls, hand weights, and pulleys.
Level one with isometric exercises is performed in a neutral, pain-free position that trains the core muscles to protect the spine. Patients are taught to strictly maintain a neutral, pain-free position, because motion through the spine during the acute, postoperative period can cause mechanical trauma and exacerbate symptoms, such as pain, weakness, or numbness. The program accelerates to an increased intensity and compromised positions with balance and coordination exercises so long as the patient is able to maintain a pain-free state. If an exercise exacerbates symptoms, the exercise is modified, decreased, or discontinued.
Proper technique is key to this program. By maintaining a neutral spine position, not only can exacerbations be avoided in the early postoperative period, but the patient can develop proper timing through proprioceptive feedback of the core muscles. The patient must be mindful to go slow and be deliberate while executing exercises. It is critical to observe feedback that might signal motion in the spine. In the beginning of this program, feedback is tactile, but becomes internal as patients advance to higher levels. Once patients achieve proper technique at level one, they are advanced through the five subsequent levels of increasing difficulty. After establishing mastery of level five, the athlete begins a series of sport-specific exercises. Ultimately, return to play depends on the following:
- Achieving the proper level of the stabilization program; for recreational golfers and tennis players, it is level three; for professional athletes, it is level five.
- Obtaining good aerobic conditioning; the key to aerobic conditioning is to diversify the aerobic exercise.
- Performing the sport-specific exercises.
- Returning slowly to the sport.
- Continuing the stabilization exercise once the athlete returns to sport.
Our trunk stabilization program has been divided into five levels of eight categories. The graduated nature of this program allows a patient to go from a neutral, pain-free position for the spine performed in a safe, controlled position, to very advanced strengthening exercises conducted in a somewhat precarious position. These exercises require higher levels of balance and coordination. The therapist’s objective is to teach the patient how to do the exercises. Regardless of how advanced the exercise may be, strict spine stability must be maintained. Often one category of exercises will advance faster than another.
PROPER TECHNIQUE FOR EIGHT EXERCISES
The therapist will advance the patient faster through exercises the patient is better able to perform, and from which the patient experiences less pain while doing. For example, in Category A, sit-ups are done with feet on the floor, back in the neutral, pain-free position, arms clasped across the chest. Then, with an elevation of the head and back, the sit-up is held briefly before returning to neutral position. The exercise is then progressively increased; weights are added to the chest, and in the final level the sit-ups are performed with arms extended forward. There is no need for the patient to fully sit up; the shoulder blades should simply be lifted until they are off the mat. Bridging exercises are done by lifting the pelvis off the floor while strictly maintaining the neutral, pain-free position. Lifting is done with the legs so the back is not arched into a hyperextended position. Holding this bridged position helps isolate trunk musculature in a different fashion than the dead bug exercises. Pain is often produced when this maneuver is performed with too much hyperextension in the lumbar spine and improper use of the gluteal muscles to stabilize the pelvis and back. This exercise is progressed through a 1-leg bridge on the ball, and weights may be added to the trunk and extended legs.
Exercises performed in the prone position challenge a patient’s ability to strictly maintain the neutral position. Initially, a cushion under the stomach can assist in avoiding movements into lumbar extension. Alternate arm and leg extensions require good trunk control to prevent hyperextension. Ball exercises provide a platform that requires a higher level of coordination and proprioceptive control to maintain strict stability. Initially, the therapist may need to provide tactile feedback to achieve this. The leg press begins with a simple balancing exercise, rolling on the ball, and maintaining control of the ball throughout the motions. Prone exercises of Supermans, swimming, and shoulder abduction challenge abdominals and gluteals to prevent hyperextension. Prayer exercises and push-ups demand upper abdominal control to maintain stability. Applying resistive forces with batons increases challenges in all planes of motion.
Wall slide exercises can begin with a gentle flexion of the knees and with no real lower extremity or back strain. This is an easy exercise initially, which can begin in the immediate postoperative period. Quadriceps strength is directly proportional to the ability to work in a bent forward position in a lifting job and, most importantly, the quadriceps exercises are a reflection of the ability of patients to use their legs rather than their backs for bending and lifting. Patients who have weak quads lock their knees and bend at the waist, which is exactly the opposite of what is desirable for a back pain patient. The wall slide progresses through a full 90°, with longer periods of holding. The addition of weights and extended arms increases the difficulty of the maneuver. The transition from the initial stage of identifying neutral position and maintaining it proceeds through a series of unsupported arm and leg motion exercises. Actively having the patient engage the abdominals and gluteals to maintain neutral spine position enhances quadriceps function and provides desired closed chain proprioceptive feedback.
Quadruped positions present unique challenges because they offer less tactile feedback. To perform quadruped positions, patients must develop better internal proprioceptive feedback mechanisms to strictly maintain neutral spine position. Patients must learn to hold this position while progressing from more simple leg or arm lifts to alternate arm and leg lifts—at first without weights, then performed with weights. Feedback in the sagittal plane must be monitored internally by the patient or assisted by therapist hand feedback.
Aerobic exercise is important for general conditioning, and choosing the right type of exercise is important. An effective strategy is diversification. Those who rely only on running or jogging may be predisposed to strains and sprains. Pool walking is an excellent solution for many patients and can commence as soon as 3 weeks postoperatively. More complex and sophisticated types of aerobic conditioning must be approached carefully. Treadmills and swimming for untrained patients can result in an exacerbation of their condition. A diversified approach to aerobic conditioning will be less likely to produce overuse syndromes. Be aware of proper technique and make sure equipment is fitted appropriately. With climbing machines and step machines, the key is to have the appropriate height step. For exercise cycles, it is important for the seat to be low enough so the feet do not reach down for the pedals, which produces rocking of the pelvis on the seat.

This structured program moves the patient’s recovery forward through a five-level program that gradually increases demands on strength, endurance, and proprioception
SCALES: A COMMON MEASURE OF PROGRESS
The functional activities levels have been expanded from the original scales to include sports activity. This modification was made to allow a greater rating for return to full sports activity. The stabilization scores, likewise, have been increased. The original three-stage scale used by Art White, MD, and Jeff Saal, MD, has been better adapted, we feel, to more intense training and stabilization exercises and allows higher levels of accomplishment for advanced exercisers and advanced stage athletes. By defining the levels of core strengthening, everyone involved in the rehabilitation process can monitor and know when the patient is able to return to activity.
The key to this program is for the patient-athlete to strictly maintain the neutral position through all exercises. Because spine motion is not allowed, patients are less likely to experience pain and injury, but, more importantly, they will develop the coordinated firing patterns of core muscles.
Robert Watkins, IV, MD, is a board-certified orthopedic spine surgeon and co-director of the Marina Spine Center at Marina Del Rey Hospital in Marina Del Rey, Calif. Dr Watkins and his father are spinal consultants for the University of Southern California, the Los Angeles Dodgers, and other Los Angeles sports teams.
Michael B. Schlink, MA, PT, OCS, is the owner of Schlink & Associates Physical Therapy, Los Angeles.
Reference
- Watkins RG, Uppal GS, Perry J, Pink M, Dinsay JM. Dynamic electromyographic analysis of trunk musculature in professional golfers. Am J Sports Med. 1996;24:535-8.