Functional electrical stimulation (FES) has been used for years to strengthen weak muscles in individuals with incomplete spinal cord injury (SCI).1-3 Studies with FES ergometry (combination FES and cycling) have demonstrated improvements in blood flow,4,5 exercise capacity,6,7 body composition,8,9 metabolism,10,11 and muscle mass8,12 in individuals with complete SCI. The full range of benefits possible with the FES bike is not clear. Furthermore, with the continual search for ways to promote neural recovery and functional gains after SCI, FES and the FES bike are regaining popularity in this population. Yet, whether FES can facilitate neural changes in individuals with SCI is even less clear.
 |
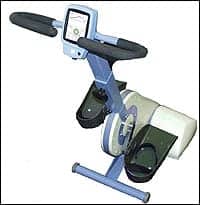
| Figure 1. S6 Ergometer System consisting of a powered cycle, FES system, and PDA controller. |
In a preliminary study evaluating a new generation of the FES bike (Figure 1), subjects with both incomplete and complete SCI at Shepherd Center have reported changes in bowel and bladder sensation and function, as well as skin integrity, blood pressure, heart rate, respiratory function, and thermoregulation, since using the FES bike.
The purpose of this study was to develop the protocol for use of the RT 300 in individuals with lower extremity (LE) paralysis due to SCI. The main goals of the study were to: 1) Evaluate subject tolerance and level of compliance with the new generation FES bike, and 2) Determine the “best” protocol for individuals with different impairments due to SCI.
The investigators’ hypotheses were that 1) Training on the new generation FES bike will result in greater health, fitness, and quality of life, as well as decreased secondary complications, in individuals with SCI; and 2) There is a “best” protocol for use, based on level of injury, and degree of motor and sensory impairment.
This study included men and women, ages 18 to 65, with acute or chronic, complete or incomplete, LE motor paralysis resulting from SCI. Individuals were excluded if they had significant health issues, such as ventilator dependence, respiratory problems, a stage II or greater pressure ulcer, or cardiac instability. Individuals were also excluded if they had severe spasticity in the LE or trunk, or significant range of motion deficits in the LE, interfering with safety on the new generation FES bike, as well as LE fractures, any other neuromuscular disorder, or lower motor neuron injury.
One novel aspect of the study was that it was designed to run as a class. All subjects used the bike together in a small area, over the span of 3 hours. This allowed one physical therapist and one or two exercise specialists to run the study. The purpose of this design was to evaluate the use of the bike with minimal therapist intervention, to make the intervention available in a cost-effective manner. Any intervention for individuals with SCI will need to span across a lifetime of recovery. If it is not affordable, then the intervention will not serve the SCI population in a long-term and meaningful way. The class format achieves this need.
After receiving approval from their physician to use the new generation FES bike, each subject was evaluated to determine neural level and completeness of injury, and response to FES. A trained physical therapist showed each subject or caregiver how and where to apply surface electrodes on each thigh and buttocks. Once they were competent with setup of the electrodes, subjects arrived with electrodes in place, and were ready to plug the electrode wires into the bike. Each subject warmed up for 2 to 4 minutes, and then started in the active mode (with electrical stimulation causing the leg muscles to contract for cycling on the bike). Subjects spent the first several sessions building up strength, endurance, and tolerance to FES. Once a subject increased endurance to the point where they were cycling for an entire hour for three sessions in a row in the active (stimulation induced cycling) mode, while maintaining an exercise rate of 40-50 revs/min, resistance was added. Resistance was incrementally increased every three sessions as tolerated. If the rpms decreased below the set level, fatigue was detected, the electrical stimulation turned off, and the motor of the new generation FES bike continued passively cycling the legs on the ergometer, so that each subject trained for a full hour each session. Subjects trained 1 hour per day, 3 days per week, for 16 weeks. Skin was checked before and after each session, and heart rate and blood pressure were monitored throughout each session.
The focus of data collection and assessment was on patient tolerance, any neural and functional changes, perception of the bike, and determining the best protocol for each subject.
 |
All subjects tolerated the electrodes, FES, and the use of the bike. There was 97% compliance in this study, with subjects missing sessions due to illness or transportation issues. One person with a C6 level of SCI, using the bike early in the recovery process (4 months post-SCI), reported immediate changes in sensation and movement below the level of injury. Some of the sensory changes assisted him with his bowel program. The most remarkable change experienced was the improvement of a skin wound on his lower leg. Prior to starting the bike, this wound seemed resistant to healing; within 2 weeks of using the bike three times a week, the wound was drying and healing. He also reported a significant increase in spasticity. Another participant (C4, 4 months post-SCI) reported marked improvements in respiratory function, whereby she was no longer short of breath when speaking. She also reported significant improvements in her quality of life, and attributed much of this to the training on the FES bike. Being that both of these people were in early stages of recovery after SCI, one cannot rule out the possibility that all of these changes would have occurred without use of the FES bike.
The reports of changes in sensation and satisfaction with the FES bike were not isolated to those with more acute injuries, however. Another woman in the study (T12, motor incomplete, 3 years post-SCI) also reported changes in sensation and strength. She reported: “One of the things that I’ve noticed after a few sessions was that my thighs were getting sore, like the soreness one would get after a good workout,” and “I also felt more tingling sensation on my right bottom.” She reported that by adding resistance to her training, she was getting a better workout and “I usually glow but I was sweating.” She also felt it was helping her sleep better.
The protocol on the new generation FES bike requires further evaluation. Some individuals on the bike were able to cycle in the active mode for the entire hour session within the first several days of using the bike. Others were unable to increase endurance using the traditional method of cycling in the active mode. These individuals were able to increase the length of time in the active mode by using a parameter called “motor assist.” This mode allowed the subject to use the motor on the bike to assist the FES in maintaining the required 40 to 50 revs/min. Typically, subjects who had not demonstrated significant improvements in endurance by the end of their first month of the study were placed on a protocol utilizing motor support. Specifically, the stimulation cycled on and off in the active mode, but the motor assisted the cycling to prevent it from switching over into passive cycling. Every three sessions, the amount of assistance from the motor was decreased until the individual was able to cycle with the stimulation only. Subjects were then progressed every three sessions as described above, adding resistance as long as revs/min were maintained. Subjects using either approach demonstrated increases in thigh girth measurements, suggesting that both approaches of progression lead to changes in the muscle. Further study is required to ascertain that the motor assist mode does not harm the muscle in any way, or that one is more or less effective for improving function.
While this early study lacks the rigor of reliable and valid outcome measures, it does suggest that the FES bike may facilitate sensory and motor changes in individuals with both complete and incomplete SCI. John McDonald and colleagues reported similar findings with an intense activity-based therapy program including the FES bike in individuals with chronic SCI.13 Although the FES bike has been shown to have health and wellness benefits, the information from this preliminary study also suggests that use of the FES bike should be reexamined for individuals with SCI, particularly with regard to neural recovery. The benefits of the FES bike for individuals with SCI may extend into areas of neural and functional recovery. If the FES bike is an effective means for improving health, wellness, neural recovery, and functional improvements, this may be an intervention to prepare individuals for locomotor training, or as an option for those for whom locomotor training is not appropriate (such as individuals with complete SCI).
Deborah Backus, PT, PhD, is the director of Spinal Cord Injury Research at Crawford Research Institute, Shepherd Center, Atlanta. Candace Rae Tefertiller, MPT, ATP, is a physical therapist at Shepherd Center.
REFERENCES
- Kralj A, Vodovnik L. Functional electrical stimulation of the extremities: part 2. J Med Eng Technol. 1977;1(2):75-80.
- Kralj A, Vodovnik L. Functional electrical stimulation of the extremities: part 1. J Med Eng Technol. 1977;1(1):12-15.
- Peckham PH. Functional electrical stimulation: current status and future prospects of applications to the neuromuscular system in spinal cord injury. Paraplegia. 1987;25:279-88.
- Nash MS, Jacobs PL, Montalvo BM, Klose KJ, Guest RS, Needham-Shropshire BM. Evaluation of a training program for persons with SCI paraplegia using the Parastep 1 ambulation system: part 5. Lower extremity blood flow and hyperemic responses to occlusion are augmented by ambulation training. Arch Phys Med Rehabil. 1997;78:808-814.
- Gerrits HL, de Haan A, Sargeant AJ, van Langen H, Hopman MT. Peripheral vascular changes after electrically stimulated cycle training in people with spinal cord injury. Arch Phys Med Rehabil. 2001;82:832-839.
- Jacobs PL, Nash MS, Klose KJ, Guest RS, Needham-Shropshire BM, Green BA. Evaluation of a training program for persons with SCI paraplegia using the Parastep 1 ambulation system: part 2. Effects on physiological responses to peak arm ergometry. Arch Phys Med Rehabil. 1997;78:794-798.
- Krauss JC, Robergs RA, Depaepe JL, et al. Effects of electrical stimulation and upper body training after spinal cord injury. Med Sci Sports Exerc. 1993;25:1054-1061.
- Klose KJ, Jacobs PL, Broton JG, et al. Evaluation of a training program for persons with SCI paraplegia using the Parastep 1 ambulation system: part 1. Ambulation performance and anthropometric measures. Arch Phys Med Rehabil. 1997;78:789-793.
- Hjeltnes N, Aksnes AK, Birkeland KI, Johansen J, Lannem A, Wallberg-Henriksson H. Improved body composition after 8 week of electrically stimulated leg cycling in tetraplegic patients. Am J Physiol. 1997;273:R1072-1079.
- Jeon JY, Weiss CB, Steadward RD, et al. Improved glucose tolerance and insulin sensitivity after electrical stimulation-assisted cycling in people with spinal cord injury. Spinal Cord. 2002;40:110-117.
- Mohr T, Dela F, Handberg A, Biering-Sorense FN, Galbo H, Kjaer M. Insulin action and long-term electrically induced training in individuals with spinal cord injuries. Med Sci Sports Exerc. 2001;33:1247-1252.
- Block JE, Steinbach LS, Friedlander AL, et al. Electrically-stimulated muscle hypertrophy in paraplegia: assessment by quantitative CT. J Comput Assist Tomogr. 1989;13:852-854
- McDonald JW, Becker D, Sadowsky CL, Jane JA Sr, Conturo TE, Schultz LM. Late recovery following spinal cord injury. Case report and review of the literature. J Neurosurg. 2002;97(2 suppl):252-65.