The Centers for Medicare & Medicaid Services (CMS) has at long last issued a national coverage decision establishing power seat elevation equipment for power wheelchairs as durable medical equipment (DME) eligible for coverage by Medicare.
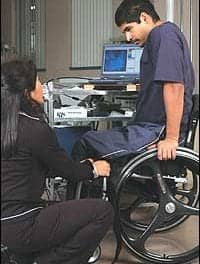
People with Medicare who perform transfers from power wheelchairs, or reach from their chair for mobility-related activities of daily living, such as dressing, grooming, toileting, feeding and bathing, can receive Medicare-covered seat elevation equipment effective immediately. This decision is expected to directly impact the quality of life for thousands of beneficiaries.
Related: CMS Releases Proposal to Expand Power Seat Elevation Equipment Coverage
After considering the public comments on the proposed decision memorandum, CMS is also expanding coverage beyond the proposed decision. CMS finds in this national coverage analysis that the evidence is sufficient to determine that power seat elevation equipment is reasonable and necessary for individuals using complex rehabilitative power-driven wheelchairs when the following conditions are met:
1. The individual has undergone a specialty evaluation that confirms the individual’s ability to safely operate the seat elevation equipment in the home. This evaluation must be performed by a licensed/certified medical professional such as a physical therapist (PT), occupational therapist (OT), or other practitioner, who has specific training and experience in rehabilitation wheelchair evaluations; and,
2. At least one of the following apply:
a. The individual performs weight bearing transfers to/from the power wheelchair while in the home, using either their upper extremities during a non-level (uneven) sitting transfer and/or their lower extremities during a sit to stand transfer. Transfers may be accomplished with or without caregiver assistance and/or the use of assistive equipment (e.g. sliding board, cane, crutch, walker, etc.); or,
b. The individual requires a non-weight bearing transfer (e.g. a dependent transfer) to/from the power wheelchair while in the home. Transfers may be accomplished with or without a floor or mounted lift; or,
c. The individual performs reaching from the power wheelchair to complete one or more mobility related activities of daily living (MRADLs) such as toileting, feeding, dressing, grooming and bathing in customary locations within the home. MRADLs may be accomplished with or without caregiver assistance and/or the use of assistive equipment.
Related: CMS Opens Consideration for Seat Elevation Systems Coverage
In addition, the Durable Medical Equipment Medicare Administrative Contractor (DME MAC) has discretion to determine reasonable and necessary coverage of power seat elevation equipment for individuals who use Medicare covered PWCs other than complex rehabilitative power-driven wheelchairs.
Related: Justifying Power Seat Elevation and Standing Systems
Standing systems have yet to be considered for coverage.